Summary
Definition
History and exam
Key diagnostic factors
- diastolic murmur
Other diagnostic factors
- dyspnea
- fatigue
- weakness
- orthopnea
- paroxysmal nocturnal dyspnea
- pallor
- mottled extremities
- rapid and faint peripheral pulse
- jugular venous distension
- basal lung crepitations
- altered mental status
- urine output <30 mL/hour
- soft S1
- soft or absent A2
- collapsing (water hammer or Corrigan) pulse
- cyanosis
- tachypnea
- displaced, hyperdynamic apical impulse
- chest pain
- pink frothy sputum
- wheeze (cardiac asthma)
- additional heart sounds
- arrhythmias
- ejection systolic flow murmur
- Austin Flint murmur
- systolic thrill
- Hill sign
- Bisferiens pulse
- de Musset sign
- Muller sign
- Traube sign
- Quincke sign
- Duroziez sign
- Mayen sign
- Lighthouse sign
- Becker sign
- Landolfi sign
- Rosenbach sign
- Gerhardt sign
- Lincoln sign
- Sherman sign
- palmar click
- syncope
Risk factors
- bicuspid aortic valve
- rheumatic fever
- endocarditis
- Marfan syndrome and related connective tissue disease
- systemic hypertension
- aortitis
- older age
Diagnostic tests
1st tests to order
- ECG
- chest x-ray
- echocardiogram
- M-mode and 2-dimensional imaging
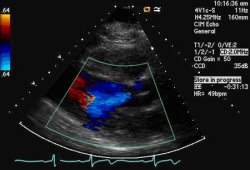
- color flow Doppler
- pulsed wave Doppler
- continuous wave Doppler
Tests to consider
- radionuclide angiography
- MRI
- exercise stress testing
- cardiac catheterization
Treatment algorithm
acute AR
chronic AR: mild to moderate
chronic AR: severe, asymptomatic
chronic AR: severe, symptomatic
Contributors
Authors
Poorna R. Karuparthi, MD, FACC
Associate Professor of Medicine
University of Missouri-Columbia
Chief of Cardiology
Harry S. Truman Veterans' Hospital
Columbia
MO
Disclosures
PRK declares that he has no competing interests.
Acknowledgements
Dr Poorna R. Karuparthi would like to gratefully acknowledge Dr Sanjeev Wasson and Dr Nishant Kalra, previous contributors to this topic.
Disclosures
SW and NK declare that they have no competing interests.
Peer reviewers
Kul Aggarwal, MD, MRCP, FACC, FACP
Professor of Clinical Medicine
University of Missouri-Columbia
Chief
Cardiology Section
Harry S. Truman Veterans Hospital
Columbia
MO
Disclosures
KA declares that he has no competing interests.
Rajdeep Khattar, DM, FRCP, FACC, FESC
Consultant Cardiologist and Honorary Senior Clinical Lecturer
Manchester Heart Centre
Central Manchester and Manchester Children's NHS Foundation Trust
Manchester
UK
Disclosures
RK declares that he has no competing interests.
John Pepper, MChir FRCS
Consultant Cardiac Surgeon
Department of Surgery
Royal Brompton Hospital
London
UK
Disclosures
JP declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Writing Committee Members, Otto CM, Nishimura RA, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021 Feb 2;77(4):e25-197.Full text Abstract
Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Mitral regurgitation (MR)
- Mitral stenosis
- Aortic stenosis
More DifferentialsGuidelines
- 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain
- 2021 ESC/EACTS guidelines for the management of valvular heart disease
More GuidelinesPatient information
Heart failure
More Patient informationVideos
Aortic regurgitation (severe)
Third heart sound gallop
More videosLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer