Summary
Definição
História e exame físico
Principais fatores diagnósticos
- chest pain
- dyspnea
- tachypnea
- presyncope or syncope
- hypotension (systolic BP <90 mmHg)
Outros fatores diagnósticos
- feeling of apprehension
- cough
- tachycardia
- fever
- unilateral swelling/tenderness of calf
- hemoptysis
- elevated jugular venous pressure
- sternal heave
- accentuated pulmonary component of S2
Fatores de risco
- diagnosis of deep vein thrombosis (DVT)
- major surgery within the preceding 3 months
- medical hospitalization within the preceding 2 months
- active cancer
- previous venous thromboembolic event
- recent trauma or fracture
- increasing age
- pregnancy and postpartum
- varicose veins
- paralysis of the lower extremities
- hereditary thrombophilias
- factor V Leiden mutation
- prothrombin G20210A mutation
- protein C and protein S deficiency
- antithrombin deficiency
- antiphospholipid antibody syndrome
- medical comorbidity
- use of specific drugs
- obesity (BMI ≥29 kg/m²)
- cigarette smoking
- recent long-duration travel
- family history of venous thromboembolism (VTE)
- central venous catheterization
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- Pulmonary Embolism Rule-Out Criteria (PERC)
- Wells criteria/Geneva score/YEARS criteria
- D-dimer test
- multiple-detector computed tomographic pulmonary angiography (CTPA)
- ventilation-perfusion (V/Q) scan
- coagulation studies
- BUN and creatinine, hepatic function tests
- CBC
Investigações a serem consideradas
- point-of-care ultrasound (POCUS)
- chest x-ray
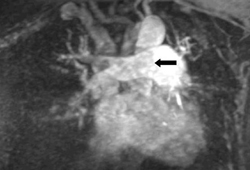
- magnetic resonance angiography (MRA)
- pulmonary angiography
- transthoracic echocardiography (TTE)
- electrocardiography (ECG)
- arterial blood gasses (ABG)
- thrombophilia screen
- ultrasonography
- troponin
Algoritmo de tratamento
high-risk (massive) PE or high clinical probability of PE with shock or hypotension (i.e., systolic BP <90 mmHg), no contraindication to anticoagulation or thrombolysis
high-risk (massive) PE or high clinical probability of PE with shock or hypotension, or intermediate-high risk, contraindication to anticoagulation or thrombolysis
intermediate-high risk, no contraindication to anticoagulation or thrombolysis
intermediate-low risk or low risk, no contraindication to anticoagulation
intermediate-low risk or low risk, contraindication to anticoagulation
confirmed PE: provoked
confirmed PE: unprovoked
confirmed PE: pregnant
confirmed PE: cancer-associated
confirmed PE: recurrent PE while on anticoagulation
Colaboradores
Consultores especialistas
Scott Stevens, MD
Director
Thrombosis Clinic
Intermountain Medical Center
Murray
Professor of Medicine
Department of Medicine
Intermountain Healthcare and University of Utah
Salt Lake City
UT
Declarações
SS declares that he has no competing interests.
Scott C. Woller, MD
Director
Thrombosis Clinic
Intermountain Medical Center
Murray
Professor
Department of Medicine
Intermountain Healthcare and University of Utah
Salt Lake City
UT
Disclosures
SCW declares that he is expecting to receive funding of an investigator initiated grant from Janssen Pharmaceuticals to Intermountain Health with no direct compensation to himself for research in the sum of $500,000 in 2024.
Gabriel V. Fontaine, PharmD, MBA, BCPS
Clinical Pharmacy Manager
Critical Care and Emergency Medicine
Advanced Clinical Pharmacist
Neuroscience Critical Care
Intermountain Medical Center
Murray
UT
Disclosures
GVF has received consulting fees and honoraria from AstraZeneca, Chiesi, and Anticoagulation Forum.
Acknowledgements
Dr Scott Stevens, Dr Scott C. Woller, and Dr Gabriel V. Fontaine would like to gratefully acknowledge Drs Geno Merli, Luis H. Eraso, Taki Galanis, Geoffrey Ouma, Miguel Angel de Gregorio, Alicia Laborda, and Seth W. Clemens, previous contributors to this topic.
Disclosures
GM has received grants or research support from BMS, J&J, Sanofi-Aventis, Portola, and Janssen; he has served as a Scientific Consultant for BMS, J&J, and Sanofi-Aventis. LHE, TG, GO, MAG, AL, and SWC declare that they have no competing interests.
Peer reviewers
Keith Wille, MD, MSPH
Associate Professor of Medicine
University of Alabama at Birmingham
Birmingham
AL
Disclosures
KW declares that he has no competing interests.
John R. Charpie, MD, PhD
Associate Professor of Pediatrics
Medical Director
Pediatric Cardiothoracic Intensive Care Unit
University of Michigan Congenital Heart Center
C.S. Mott Children's Hospital
Ann Arbor
MI
Disclosures
JRC declares that he has no competing interests.
Sanjeev Wasson, MD
Advanced Clinical Fellow
Cleveland Clinic Foundation
Cleveland
OH
Disclosures
SW declares that he has no competing interests.
David Jimenez, MD, PhD
Respiratory Physician and Associate Professor
Ramón y Cajal Hospital and Alcalá de Henares University
Respiratory Department and Medicine Department
Madrid
Spain
Disclosures
DJ has received consulting fees from Boehringer Ingelheim, Bayer, Leo-Pharm, and Rovi, and lecture fees from Sanofi Aventis.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Konstantinides SV, Meyer G, Becattini C, et al. 2019 ESC guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS). Eur Heart J. 2020 Jan 21;41(4):543-603.Full text
Stevens SM, Woller SC, Baumann Kreuziger L, et al. Antithrombotic therapy for VTE disease: second update of the CHEST guideline and expert panel report. 2021 Dec;160(6):e545-608.Full text Abstract
American College of Radiology. ACR appropriateness criteria: suspected pulmonary embolism. 2022 [internet publication].Full text
Bates SM, Rajasekhar A, Middeldorp S, et al. American Society of Hematology 2018 guidelines for management of venous thromboembolism: venous thromboembolism in the context of pregnancy. Blood Adv. 2018 Nov 27;2(22):3317-59.Full text Abstract
Stevens SM, Woller SC, Baumann Kreuziger L, et al. Antithrombotic therapy for VTE disease: compendium and review of CHEST guidelines 2012-2021. Chest. 2024 Aug;166(2):388-404.Full text Abstract
Lyman GH, Carrier M, Ay C, et al. American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood Adv. 2021 Feb 23;5(4):927-74.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Angina, unstable
- Myocardial infarction, non-ST elevation (NSTEMI)
- Myocardial infarction, ST elevation (STEMI)
More DifferentialsGuidelines
- ACR appropriateness criteria: management of acute pulmonary embolism
- NCCN clinical practice guidelines in oncology: cancer-associated venous thromboembolic disease
More GuidelinesCalculators
Pulmonary Embolism Wells Score
Revised Geneva Score for Estimation of the Clinical Probability of Pulmonary Embolism in Adults
More CalculatorsVideos
Tracheal intubation: animated demonstration
Bag-valve-mask ventilation: animated demonstration
More videosPatient information
Pulmonary embolism: what is it?
Deep vein thrombosis
Más Patient informationInicie sesión o suscríbase para acceder a todo el BMJ Best Practice
El uso de este contenido está sujeto a nuestra cláusula de exención de responsabilidad