Summary
Definición
Anamnesis y examen
Principales factores de diagnóstico
- abdominal pain
- nausea and vomiting
- anorexia
- signs of hypovolemia
Otros factores de diagnóstico
- signs of organ dysfunction
- Grey-Turner sign
- Cullen sign
- Fox sign
- abdominal distention
Factores de riesgo
- middle-aged women
- young- to middle-aged men
- gallstones
- alcohol
- hypertriglyceridemia
- hypercalcemia
- use of causative drugs
- mumps
- coxsackievirus
- Mycoplasma pneumoniae
- endoscopic retrograde cholangiopancreatography (ERCP)
- trauma
- pancreas divisum
- pancreatic cancer
- sphincter of Oddi dysfunction
- family history of pancreatitis
Pruebas diagnósticas
Primeras pruebas diagnósticas para solicitar
- serum lipase (or amylase if lipase is unavailable)
- liver function tests
- CBC and differential
- hematocrit
- BUN and serum electrolytes
- arterial blood gas
- CRP
- transabdominal ultrasound
- chest x-ray
- ratio of serum lipase:amylase
- serum triglycerides
Pruebas diagnósticas que deben considerarse
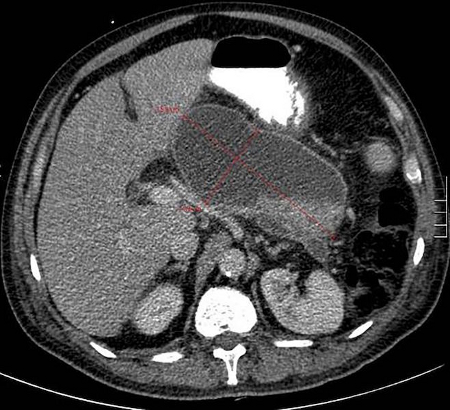
- abdominal CT scan
- magnetic resonance imaging/magnetic resonance cholangiopancreatography (MRI/MRCP)
- endoscopic ultrasound (EUS)
Pruebas emergentes
- procalcitonin
Algoritmo de tratamiento
all patients
deteriorating or failing to improve
Colaboradores
Consejeros especializados
Scott Tenner, MD, MPH, JD, FACG
Clinical Professor of Medicine
Director, The Greater New York Endoscopy Surgical Center
Director, Brooklyn Gastroenterology and Endoscopy
State University of New York
NY
Divulgaciones
ST is an author of references cited in this topic. He declares that he has no other competing interests.
Craig T. Tenner, MD, FACP
Associate Professor
Medicine
New York University School of Medicine
NY
Divulgaciones
CTT declares that he has no competing interests.
Agradecimientos
Dr Scott Tenner and Dr Craig T. Tenner would like to gratefully acknowledge Dr Nicholas J. Zyromski, Dr Brian Daley, Dr Catherine Lindsay McKnight, and Dr Fernando Aycinena, previous contributors to this topic. They would also like to thank Dr Camille Blackledge for her contribution to this topic.
Divulgaciones
NJZ is an author of a reference cited in this topic. BD, CLM, FA, and CB declare that they have no competing interests.
Revisores por pares
Tamas A. Gonda, MD
Assistant Professor of Medicine
Attending Physician and Director of Research
Columbia University Medical Center
New York
NY
Divulgaciones
TAG declares that he has no competing interests.
Alan Moss, MD
Harvard Medical Faculty Physician
Division of Gastroenterology
Beth Israel Deaconess Medical Center
Boston
MA
Divulgaciones
AM declares that he has no competing interests.
Derek O'Reilly, MD
Consultant Hepatobiliary & Pancreatic Surgeon
Department of Surgery
North Manchester General Hospital
Manchester
UK
Divulgaciones
DOR is an author of a reference cited in this topic. He declares that he has no other competing interests.
Eric Frykberg, MD
Professor
Department of Surgery
Division General Surgery
Shands Jacksonville Medical Center
FL
Declarações
At the time of the peer review, Dr E. Frykberg declared no competing interests. We were made aware that Dr Frykberg is now deceased.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Tenner S, Vege S, Sheth S, et al. American College of Gastroenterology guidelines: management of acute pancreatitis. Am J Gastroenterol. 2024 Mar 119(3):419-37.Texto completo Resumo
Leppäniemi A, Tolonen M, Tarasconi A, et al. 2019 WSES guidelines for the management of severe acute pancreatitis. World J Emerg Surg. 2019 Jun 13;14:27.Texto completo Resumo
Working Group IAP/APA Acute Pancreatitis Guidelines. IAP/APA evidence-based guidelines for the management of acute pancreatitis. Pancreatology. 2013 Jul-Aug;13(4 Suppl 2):e1-15.Texto completo Resumo
American College of Radiology. ACR appropriateness criteria: acute pancreatitis. 2019 [internet publication].Texto completo
Crockett SD, Wani S, Gardner TB, et al. American Gastroenterological Association Institute guideline on initial management of acute pancreatitis. Gastroenterology. 2018 Mar;154(4):1096-101.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Peptic ulcer disease
- Perforated viscus
- Esophageal spasm
Mais Diagnósticos diferenciaisDiretrizes
- American College of Gastroenterology guidelines: management of acute pancreatitis
- American College of Gastroenterology guidelines: management of acute pancreatitis
Mais DiretrizesVideos
Venepuncture and phlebotomy: animated demonstration
Radial artery puncture animated demonstration
Mais vídeosFolhetos informativos para os pacientes
Pancreatitis, acute
Pancreatic cancer
Mais Folhetos informativos para os pacientesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer