Summary
Definition
History and exam
Key diagnostic factors
- past history of unexplained cardiac arrest or documented PMVT or VF
- cardiogenic syncope
Other diagnostic factors
- inducible features of Brugada syndrome (BrS)
- atrial arrhythmias
- nocturnal agonal respirations
Risk factors
- age 30 to 50 years
- male sex
- Asian ancestry
- family history of Brugada syndrome (BrS) or suspicious or unexplained cardiac death
Diagnostic investigations
1st investigations to order
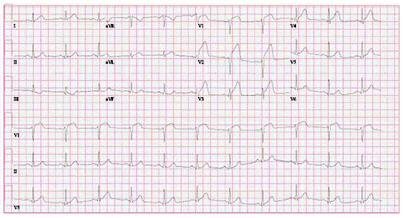
- ECG
- echocardiogram
Investigations to consider
- provocative drug testing with sodium channel blockade
- genetic testing for BrS
- advanced cardiac imaging (MRI or CT)
- invasive electrophysiological (EP) study with inducibility testing for ventricular arrhythmias
Treatment algorithm
with acute ventricular arrhythmia
asymptomatic
symptomatic
Contributors
Authors
Eugene H Chung, MD, MPH
Professor of Internal Medicine
Director of Sports Electrophysiology Clinic
Massachusetts General Hospital
Harvard Medical School
Boston
MA
Disclosures
EHC declares that he has no competing interests.
Acknowledgements
Professor Eugene H Chung would like to gratefully acknowledge Dr Mohammed-Ali Jazayeri for his contribution to the initial drafts of this topic.
Disclosures
MAJ declares that he has no competing interests.
Peer reviewers
Sei Iwai, MD
Section Chief, Cardiac Electrophysiology
Department of Cardiology
Westchester Medical Center Health Network
Valhalla
NY
Disclosures
SI declares that he has no competing interests.
Amanda Varnava, MA(Hons), MD, FRCP
Consultant Cardiologist
Imperial College Healthcare Trust
London
UK
Disclosures
AV declares that she has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Krahn AD, Behr ER, Hamilton R, et al. Brugada syndrome. JACC Clin Electrophysiol. 2022 Mar;8(3):386-405.Full text Abstract
Cronin EM, Bogun FM, Maury P, et al. 2019 HRS/EHRA/APHRS/LAHRS expert consensus statement on catheter ablation of ventricular arrhythmias. Europace. 2019 Aug 1;21(8):1143-4.Full text Abstract
Priori SG, Wilde AA, Horie M, et al. HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes: document endorsed by HRS, EHRA, and APHRS in May 2013 and by ACCF, AHA, PACES, and AEPC in June 2013. Heart Rhythm. 2013;10(12):1932-63.Full text Abstract
Zeppenfeld K, Tfelt-Hansen J, de Riva M, et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022 Oct 21;43(40):3997-4126.Full text Abstract
Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: Executive summary: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Heart Rhythm. 2018 Oct;15(10):e190-e252.Full text Abstract
Priori SG, Wilde AA, Horie M, et al. Executive summary: HRS/EHRA/APHRS expert consensus statement on the diagnosis and management of patients with inherited primary arrhythmia syndromes. Heart Rhythm. 2013;10(12):e85-108.Full text Abstract
Nielsen JC, Lin YJ, de Oliveira Figueiredo MJ, et al. European Heart Rhythm Association (EHRA)/Heart Rhythm Society (HRS)/Asia Pacific Heart Rhythm Society (APHRS)/Latin American Heart Rhythm Society (LAHRS) expert consensus on risk assessment in cardiac arrhythmias: use the right tool for the right outcome, in the right population. J Arrhythm. 2020 Jun 15;36(4):553-607.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Acute coronary syndrome
- Arrhythmogenic cardiomyopathy
- Athlete’s heart
More DifferentialsGuidelines
- 2022 ESC guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death
- 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer