Summary
Definition
History and exam
Key diagnostic factors
- abdominal pain
- anorexia
- nausea and vomiting
- right lower quadrant tenderness
- tense rigid abdomen
- hypotension and tachycardia
- palpable mass
Other diagnostic factors
- age of occurrence
- fever
- flushed face and a fetor
- diminished bowel sounds
- tachycardia
- loose stool
- constipation
- Rovsing sign
- psoas sign
- obturator sign
Risk factors
- differences in the appendiceal microbiome
- smoking
Diagnostic tests
1st tests to order
- CBC
- CRP
- abdominal and pelvic CT scan
Tests to consider
- abdominal ultrasound
- urinalysis
- urinary pregnancy test
- abdominal and pelvic MRI in pregnancy
Emerging tests
- Neutrophil-to-lymphocyte ratio
- serum sodium
- pentraxin-3
- serum amyloid A
- platelet indices
Treatment algorithm
uncomplicated acute appendicitis
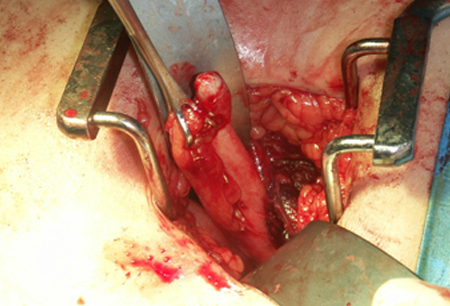
ill with perforation or abscess
Contributors
Expert advisers
Peter Szasz, MD, PhD, FRCSC
Assistant Professor
Department of Surgery
Queen's University
Kingston
Ontario
Canada
Disclosures
PS declares that he has no competing interests.
Elisabeth Adderson, MD
Associate Member
St. Jude Children's Research Hospital
Associate Professor of Pediatrics
University of Tennessee Health Sciences Center
Memphis
TN
Disclosures
EA declares that she has no competing interests.
Peer reviewers
John M. Davis, MD
General Surgery
Jersey Shore Medical Center
Neptune
NJ
Disclosures
JMD declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Di Saverio S, Podda M, De Simone B, et al. Diagnosis and treatment of acute appendicitis: 2020 update of the WSES Jerusalem guidelines. World J Emerg Surg. 2020 Apr 15;15(1):27.Full text Abstract
American College of Radiology. ACR appropriateness criteria: right lower quadrant pain - suspected appendicitis. 2022 [internet publication].Full text
Sartelli M, Chichom-Mefire A, Labricciosa FM, et al. The management of intra-abdominal infections from a global perspective: 2017 WSES guidelines for management of intra-abdominal infections. World J Emerg Surg. 2017 Jul 10;12:29.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Acute mesenteric adenitis
- Viral gastroenteritis
- Meckel diverticulitis
More DifferentialsGuidelines
- SAGES guideline for the diagnosis and treatment of appendicitis
- Acute abdominal pain
More GuidelinesCalculators
APACHE II scoring system
More CalculatorsVideos
Venepuncture and phlebotomy: animated demonstration
Peripheral intravascular catheter: animated demonstration
More videosPatient information
Appendicitis
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer