Summary
Definition
History and exam
Key diagnostic factors
- patient unresponsive
- absence of normal breathing
- absence of circulation
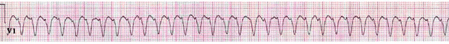
- cardiac rhythm disturbance
Risk factors
- coronary artery disease (CAD)
- left ventricular dysfunction
- age
- hypertrophic cardiomyopathy (HCM)
- arrhythmogenic right ventricular dysplasia (ARVD)
- long QT syndrome (LQTS)
- medications that prolong the QT interval or cause electrolyte disturbances
- acute medical or surgical emergency
- poisoning
- Brugada syndrome
- valvular heart disease
- smoking
- history of eating disorders
Diagnostic tests
1st tests to order
- continuous cardiac monitoring
- CBC
- serum electrolytes
- ABG
- cardiac biomarkers
- point of care ultrasound (POCUS)
Tests to consider
- ECG
- coronary angiography
- echocardiogram
- exercise stress testing
- chest x-ray
- toxicology screen
- cardiac magnetic resonance imaging
- coronary computed tomography angiography
- signal-averaged ECG (SAECG)
- electrophysiologic study
Treatment algorithm
unwitnessed cardiac arrest
shockable rhythms (pulseless ventricular tachycardia or ventricular fibrillation)
nonshockable rhythms (pulseless electrical activity or asystole)
return of spontaneous circulation
no return of spontaneous circulation
Contributors
Authors
John Wink, MD
Emergency Physician
Alberta Health Services
Alberta
Canada
Disclosures
JW declares that he has no competing interests.
Eddy Lang, MD
Professor and Department Head of Emergency Medicine
Cumming School of Medicine
University of Calgary
Alberta Health Services
Calgary
Canada
Disclosures
EL declares that he has no competing interests.
Acknowledgements
Dr John Wink and Professor Eddy Lang would like to gratefully acknowledge Dr Amar Krishnaswamy and Dr Arman T. Askari, previous contributors to this topic.
Disclosures
AK and ATA declare that they have no competing interests.
Peer reviewers
Vaikom Mahadevan, MD
Professor of Medicine
Division of Cardiology
University of California
San Francisco
CA
Declarações
VM declares that he has no competing interests.
Anthony Aizer, MD, MS
Instructor
NYU Department of Medicine (Cardiology)
Leon H Charney Heart Rhythm Center and New York University
New York
NY
Declarações
AA declares that he has no competing interests.
Massimo F. Piepoli, MD, PhD, FESC
Honorary Clinical Senior Lecturer/Consultant
Department of Cardiology
Imperial College London
London
UK
Declarações
MFP declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Panchal AR, Bartos JA, Cabañas JG, et al. Part 3: adult basic and advanced life support: 2020 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2020 Oct 20;142(16_suppl_2):S366-468.Texto completo Resumo
Martin SS, Aday AW, Allen NB, et al. 2025 heart disease and stroke statistics: a report of US and global data from the American Heart Association. Circulation. 2025 Feb 25;151(8):e41-660.Texto completo Resumo
Zeppenfeld K, Tfelt-Hansen J, de Riva M, et al. 2022 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Eur Heart J. 2022 Oct 21;43(40):3997-4126.Texto completo Resumo
Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death. Circulation. 2018 Sep 25;138(13):e272-391.Texto completo Resumo
Greif R, Bray JE, Djärv T, et al. 2024 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations: summary from the basic life support; advanced life support; pediatric life support; neonatal life support; education, implementation, and teams; and first aid task forces. Resuscitation. 2024 Dec;205:110414.Texto completo Resumo
Nolan JP, Sandroni C, Böttiger BW, et al. European Resuscitation Council and European Society of Intensive Care Medicine guidelines 2021: post-resuscitation care. Intensive Care Med. 2021 Apr;47(4):369-421.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diretrizes
- Critical care management of patients after cardiac arrest: a scientific statement from the American Heart Association and Neurocritical Care Society
- 2024 International consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations
Mais DiretrizesFolhetos informativos para os pacientes
Heart attack: what is it?
Bag-valve-mask ventilation
Mais Folhetos informativos para os pacientesVideos
Radial artery puncture animated demonstration
Femoral artery puncture animated demonstration
More vídeosLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer
