Summary
Definition
History and exam
Key diagnostic factors
- symptoms of anemia
- splenomegaly
Other diagnostic factors
- childhood or young adulthood
- family history of alpha-thalassemia
- symptoms of gallstones
- growth retardation
- history of prior iron supplementation
- jaundice
- mild dysmorphic facial features
- extramedullary hematopoiesis
Risk factors
- ethnicity from a geographic malarial area
- positive family history
Diagnostic tests
1st tests to order
- hemoglobin (Hb)
- mean corpuscular volume (MCV)
- mean corpuscular hemoglobin (MCH)
- red blood cell count
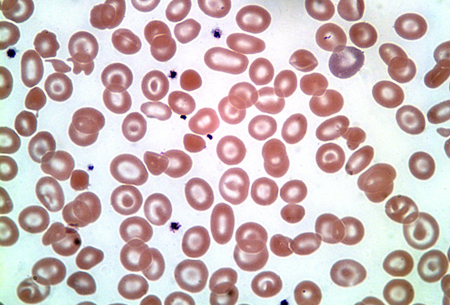
- peripheral smear
- reticulocyte percentage
- serum iron
- serum ferritin
Tests to consider
- brilliant cresyl blue staining of red blood cells
- Hb electrophoresis
- Hb fractionation by high-performance liquid chromatography (HPLC)
- gap-polymerase chain reaction (gap-PCR)
- multiplex ligation-dependent probe amplification
- direct sequencing/reverse dot blot
- MRI (hepatic or cardiac)
- superconducting quantum interference devices (SQUID)
- liver biopsy
Treatment algorithm
acute hemolytic episodes: pregnant or nonpregnant
transient aplastic crisis: pregnant or nonpregnant
nonpregnant
pregnant
Contributors
Authors
Janet L. Kwiatkowski, MD, MSCE
Director
Thalassemia Program
Children’s Hospital of Philadelphia
Professor of Pediatrics
Perelman School of Medicine
University of Pennsylvania
Philadelphia
PA
Disclosures
JLK has participated in research trials of gene therapy sponsored by bluebird bio, Sangamo, Vertex, and Editas, and has participated in studies of pyruvate kinase activators sponsored by Agios and Forma Therapeutics. She has consulted for Agios, Forma, NovoNordisk, Chiesi, Biomarin, Regeneron, Vertex, and Bristol Myers Squibb (Celgene).
Acknowledgements
Dr Janet L. Kwiatkowski would like to gratefully acknowledge Dr Elizabeth A. Price and Dr Stanley L. Schrier, the previous contributors to this topic.
Disclosures
EAP declares that she has no competing interests. SLS has received National Institutes of Health (NIH) research funds, has received funds for organizing an educational symposium, and is an author of a number of references cited in this topic.
Peer reviewers
David H. K. Chui, MD, FRCPC
Professor of Medicine
Boston University School of Medicine
Boston
MA
Disclosures
DHKC is an author of a number of references cited in this topic. He has received research grants or salary from the US National Institutes of Health greater than 6 figures USD.
Piero Giordano, PhD
Professor of Clinical Biochemical Molecular Genetics
Human and Clinical Genetics Department
Leiden University Medical Center
Leiden
The Netherlands
Disclosures
PG declares that he has no competing interests.
Cornelis Harteveld, PhD
Clinical Molecular and Biochemical Geneticist
Department of Clinical Genetics
Leiden University Medical Center
Leiden
The Netherlands
Disclosures
CH declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Thalassaemia International Federation. Guidelines for the management of alpha-thalassaemia (2023). 2023 [internet publication].Full text
Northern California Comprehensive Thalassemia Center. Standards of care guidelines for thalassemia. 2012 [internet publication].Full text
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Iron-deficiency anemia
- Beta-thalassemia
- Variant hemoglobins (Hb E, Hb Lepore)
More DifferentialsGuidelines
- Guidelines for the management of alpha-thalassaemia (2023)
- Hemoglobinopathies in pregnancy: practice advisory
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer