Summary
Differentials
Common
- Lumbar muscular strain/sprain
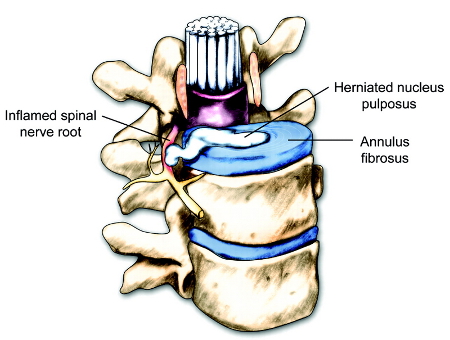
- Herniated nucleus pulposus
- Spinal stenosis
- Compression fracture
- Degenerative disk disease or facet arthropathy
- Sacroiliitis
Uncommon
- Cauda equina syndrome
- Spinal cord compression
- Spondylolysis and/or spondylolisthesis
- Vertebral discitis/osteomyelitis
- Malignancy
- Inflammatory spondyloarthropathy
- Connective tissue disease
- Scoliosis
- Abdominal aortic aneurysm
- Acute pancreatitis
- Pyelonephritis
- Renal colic
- Peptic ulcer disease
- Spinal epidural abscess
- Herpes zoster infection
- Retroperitoneal bleed
Contributors
Authors
Daniel K. Park, MD

Professor
Department of Orthopedic Surgery
William Beaumont Hospital
Royal Oak
MI
Disclosures
DKP is a consultant for Stryker, Arthrex, Medynus, Orthofix, Atlas Spine, and Amplify.
Kern Singh, MD

Professor
Department of Orthopedic Surgery
Rush University Medical Center
Chicago
IL
Disclosures
KS has received royalties from Zimmer, Stryker, RTI Surgical, Lippincott Williams & Wilkins, Thieme, Jaypee Publishing, and Slack Publishing. He holds stock in Avaz Surgical LLC, and Vital 5 LLC, has consulted for Depuy, Zimmer, K2M, and Stryker, is a board member of Vital 5 LLC, TDi LLC, Minimally Invasive Spine Study Group, is on the board of directors for CSRS, ISASS, AAOS, and is on the editorial board for Contemporary Spine Surgery and Orthopedics Today. KS has received a CSRS resident grant.
Acknowledgements
Dr Daniel K. Park and Dr Kern Singh would like to gratefully acknowledge Dr Howard S. An, a previous contributor to this topic.
Disclosures
HSA declares that he has no competing interests.
Peer reviewers
Eric L. Matteson, MD
Professor of Medicine
Mayo Clinic College of Medicine
Division of Rheumatology
Rochester
MN
Disclosures
ELM declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management. Dec 2020 [internet publication].Full text
American College of Radiology. ACR appropriateness criteria: low back pain. 2021 [internet publication].Full text Abstract
American College of Radiology. ACR appropriateness criteria: acute spinal trauma. 2024 [internet publication].Full text
American College of Radiology. ACR appropriateness criteria: inflammatory back pain: known or suspected axial spondyloarthritis. 2021 [internet publication].Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Patient information
Back pain (lower back)
Slipped disk (lower back): what is it?
More Patient informationVideos
Inspection of the back
Physical examination of the back demonstration
More videosLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer