Summary
Definition
History and exam
Key diagnostic factors
- chest pain
- diaphoresis
- cardiogenic shock
- acute heart failure
Other diagnostic factors
- nausea and vomiting
- epigastric pain
- arrhythmias
- abnormal heart sounds
- shortness of breath
- syncope
- early morning onset
Risk factors
- smoking
- hypertension
- diabetes
- obesity and metabolic syndrome phenotype
- sedentary behavior and physical inactivity
- dyslipidemia
- chronic kidney disease (CKD)
- atherosclerosis (history of angina, myocardial infarction, stroke, transient ischemic attack, peripheral vascular disease)
- family history of premature coronary artery disease (CAD)
- age >60 years
- cocaine use
- depression
- stent thrombosis or restenosis
- sleep apnea
- surgical procedures (including intraoperative and postoperative periods)
- migraine
- adverse pregnancy outcomes
- anticholinergic burden
Diagnostic tests
1st tests to order
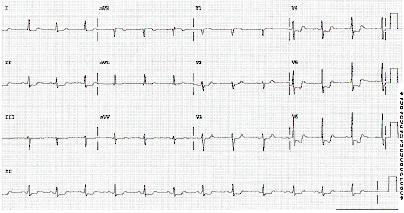
- ECG
- cardiac biomarkers
- echocardiography
- CXR
- CBC
- BUN and serum creatinine
- electrolytes
- LFTs
- blood glucose
- CRP
Tests to avoid
- coronary artery calcium (CAC)
Tests to consider
- angiography/cardiac catheterization
- lipids
- brain natriuretic peptide (BNP) or N-terminal pro-BNP (NT-pro-BNP)
- stress testing
- coronary CT angiography (CCTA)
Treatment algorithm
acute presentation
post-stabilization
Contributors
Expert advisers
Mahi L. Ashwath, MD, MBA, FACC, FASE, FSCMR
Professor of Medicine and Radiology
Multimodality Imaging Director
Inaugural Reuben Jacobs Chair in Internal Medicine
UHS/UT Heart and Vascular Institute
San Antonio
TX
Disclosures
MLA declares that she is a consultant for Tersera.
Acknowledgements
Dr Mahi L. Ashwath would like to gratefully acknowledge Dr Sanjay Gandhi, Dr Cody Deen, Dr Sripal Bangalore, Dr Mina Owlia, Dr Thomas Vanhecke, and Dr Dena Krishnan, the previous contributors to this topic.
Disclosures
SG declares that he is Senior Director of Medical Strategy and Innovation for the US market at Philips. SG is a senior advisor at Emeritus. SG is a voluntary board member of the American College of Cardiology (ACC) National Cardiovascular Data Registry oversight committee, the Chest Pain Myocardial Infarction registry steering committee, and the ACC finance committee. CSD was previously the Director of Cardiac Rehab for Chatham Hospital, which was financially set up as a consultancy relationship, until 2017. CSD has spoken (unpaid) at the Update in Cardiology and Update in Internal Medicine Conferences at UNC for the last 5 years. CSD has served as the PI for the Dal-GeneE (site now closed) and the ACCELERATE Trials at the University of North Carolina (trial now completed). Each trial required paid travel to an investigator meeting. SB, MO, TV, and DK declare that they have no competing interests.
Peer reviewers
Syed Wamique Yusuf, MBBS, FRCPI
Professor of Medicine
Department of Cardiology
University of Texas
MD Anderson Cancer Center
Houston
TX
Disclosures
SWY declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Rao SV, O'Donoghue ML, Ruel M, et al. 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2025 Apr;151(13):e771-862.Full text Abstract
Thygesen K, Alpert JS, Jaffe AS, et al; Executive Group on behalf of the Joint European Society of Cardiology (ESC)/American College of Cardiology (ACC)/American Heart Association (AHA)/World Heart Federation (WHF) Task Force for the Universal Definition of Myocardial Infarction. Fourth universal definition of myocardial infarction (2018). J Am Coll Cardiol. 2018 Oct 30;72(18):2231-64.Full text Abstract
Byrne RA, Rossello X, Coughlan JJ, et al. 2023 ESC guidelines for the management of acute coronary syndromes. Eur Heart J. 2023 Oct 12;44(38):3720-826.Full text
Writing Committee Members; Gulati M, Levy PD, Mukherjee D, et al. 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain: a report of the American College of Cardiology/American Heart Association Joint Committee On Clinical Practice Guidelines. J Am Coll Cardiol. 2021 Nov 30;78(22):e187-285.Full text Abstract
Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014 Dec 23;64(24):e139-228.Full text Abstract
Lawton JS, Tamis-Holland JE, Bangalore S, et al. 2021 ACC/AHA/SCAI guideline for coronary artery revascularization: a report of the American College of Cardiology/American Heart Association Joint Committee On Clinical Practice Guidelines. Circulation. 2022 Jan 18;145(3):e18-114.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- ST-elevation myocardial infarction (STEMI)
- Unstable angina
- Aortic dissection
More DifferentialsGuidelines
- 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines
- 2025 ACC/AHA/ACEP/NAEMSP/SCAI guideline for the management of patients with acute coronary syndromes
More GuidelinesCalculators
ASCVD Risk Estimator Plus
ASCVD Risk Estimator Plus
More CalculatorsPatient information
Heart attack
Heart attack: what is it?
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer