Summary
Definition
History and exam
Key diagnostic factors
- splenomegaly
- fatigue
- malaise
- night sweats
- fever
- abnormal/excessive bleeding
- bone pain
Other diagnostic factors
- weight loss
- petechiae, ecchymoses, or easy bruising
- infection
- abdominal pain
- visual changes
- focal neurologic signs
- priapism
- tinnitus
- confusion or stupor
Risk factors
- history of chronic myeloid leukemia (CML)
- exposure to alkylating chemotherapeutic agents
- exposure to ionizing radiation
Diagnostic tests
1st tests to order
- CBC and differential
Tests to consider
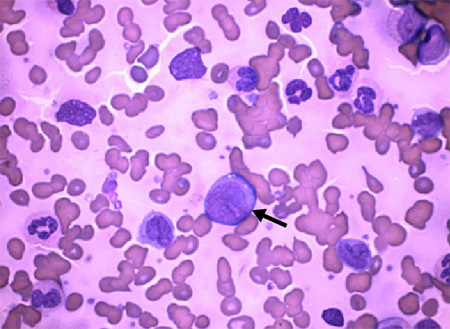
- peripheral blood smear
- bone marrow aspiration and biopsy for cytogenetic analysis
- quantitative reverse-transcriptase polymerase chain reaction (qRT-PCR)
- fluorescence in situ hybridization
- flow cytometry
- mutational analysis
- HLA1 testing
- lumbar puncture
- serum leukocyte alkaline phosphatase
- serum vitamin B12
Treatment algorithm
lymphoid blast crisis
myeloid blast crisis
biphenotypic blast crisis
suboptimal response to initial treatment
partial hematologic response or second chronic phase
transplant failure or recurrence posttransplant
Contributors
Authors
Carlos Palacio, MD, MPH, FACP
Professor of Medicine
University of Florida College of Medicine
Jacksonville
FL
Disclosures
CP declares that he has no competing interests.
Marwan E. Shaikh, MD
Assistant Professor
College of Medicine
Division of Hematology and Oncology
Mayo Clinic Jacksonville
Jacksonville
FL
Disclosures
MES declares that he has no competing interests.
Acknowledgements
Dr Carlos Palacio and Dr Marwan E. Shaikh would like to gratefully acknowledge Fauzia Rana, a previous contributor to this topic.
Disclosures
FR declares that she has no competing interests.
Peer reviewers
Danilo Perrotti, MD, PhD
Assistant Professor of Human Cancer Genetics
Ohio State University
Columbus
OH
Disclosures
DP declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: chronic myeloid leukemia [internet publication].Full text
Smith G, Apperley J, Milojkovic D, et al; British Society for Haematology. A British Society for Haematology guideline on the diagnosis and management of chronic myeloid leukaemia. Br J Haematol. 2020 Oct;191(2):171-93.Full text Abstract
Hochhaus A, Saussele S, Rosti G, et al; ESMO Guidelines Committee. Chronic myeloid leukaemia: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2017 Jul 1;28(suppl 4):iv41-51.Full text Abstract
Hochhaus A, Baccarani M, Silver RT, et al. European LeukemiaNet 2020 recommendations for treating chronic myeloid leukemia. Leukemia. 2020 Apr;34(4):966-84.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Organ-specific or systemic infection (bacterial, fungal, viral)
- Leukemoid reaction
- Essential thrombocythemia
More DifferentialsGuidelines
- Chronic myeloid leukemia
- NCCN clinical practice guidelines in oncology: hematopoietic cell transplantation (HCT)
More GuidelinesLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer