Summary
Diagnósticos diferenciais
comuns
- Corneal ulcer
- Dry eye syndrome (tear dysfunction syndrome)
- Dry age-related macular degeneration
- Uveitis/scleritis
- Cataract
- Nondiabetic myopic lens shift
- Wet age-related macular degeneration
- Vitreous hemorrhage
- Retinal venous occlusion
- Retinal arterial occlusion
- Stroke
- Migraine headache or migraine aura without headache (acephalgic migraine)
- Pituitary tumor
- Diabetic retinopathy
- Diabetic myopic lens shift
Incomuns
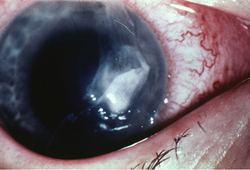
- Corneal hydrops
- Traumatic vision loss
- Optic neuritis
- Papilledema
- Leber hereditary optic neuropathy (LHON)
- Acute angle-closure glaucoma
- Retinal detachment
- Postoperative endophthalmitis
- Central retinal artery occlusion
- Pituitary apoplexy
- Arteritic anterior ischemic optic neuropathy/giant cell arteritis
- Nonarteritic anterior ischemic optic neuropathy
- Transient ischemic attack (TIA)
- Cancer-associated retinopathy
Colaboradores
Autores
Jeffrey R. SooHoo, MD, MBA
Associate Professor
Sue Anschutz-Rodgers Eye Center
Department of Ophthalmology
University of Colorado School of Medicine
Aurora
CO
Declarações
JRS declares that he has no competing interests.
Agradecimentos
Dr Jeffrey R. SooHoo would like to gratefully acknowledge Dr Prem S. Subramanian, the previous contributor to this topic.
Declarações
PSS declares that he has no competing interests.
Revisores
Andrew G. Lee, MD
The H. Stanley Neuro-ophthalmology Professor of Ophthalmology, Neurology, and Neurosurgery
The University of Iowa Hospitals and Clinics
Iowa City
IA
Declarações
AGL declares that he has no competing interests.
Robert Avery, MD, PhD
Professor of Ophthalmology
University of New Mexico Medical School
Albuquerque
NM
Declarações
RA declares that he has no competing interests.
Augusto Azuara-Blanco, PhD, FRCS(Ed), FRCOphth
Clinical Senior Lecturer
Health Services Research Unit
University of Aberdeen
Honorary Consultant Ophthalmologist
NHS Grampian
Aberdeen
UK
Declarações
AA-B declares that he has no competing interests.
Stephen Vernon, DM, FRCS, FRCOphth, FCOptom (Hon), DO
Special Professor of Ophthalmology
University of Nottingham
Consultant Ophthalmic Surgeon
Nottingham University Hospitals
Nottingham
UK
Declarações
None declared.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Rossi T, Boccassini B, Iossa M, et al. Triaging and coding ophthalmic emergency: the Rome Eye Scoring System for Urgency and Emergency (RESCUE): a pilot study of 1,000 eye-dedicated emergency room patients. Eur J Ophthalmol. 2007 May-Jun;17(3):413-7. Resumo
Bird AC, Bressler NM, Bressler SB, et al. An international classification and grading system for age-related maculopathy and age-related macular degeneration. Surv Ophthalmol. 1995 Mar-Apr;39(5):367-74. Resumo
Donahue SP, Baker CN; American Academy of Pediatrics; American Association of Certified Orthoptists; American Association for Pediatric Ophthalmology and Strabismus; American Academy of Ophthalmology. Procedures for the evaluation of the visual system by pediatricians. Pediatrics. 2016 Jan;137(1). (Reaffirmed Feb 2022).Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Folhetos informativos para os pacientes
Glaucoma
Herpes simplex eye infection
Mais Folhetos informativos para os pacientesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal