Summary
Definition
History and exam
Key diagnostic factors
- watery discharge
- ropy, mucoid discharge
- purulent discharge
- itching predominant symptom
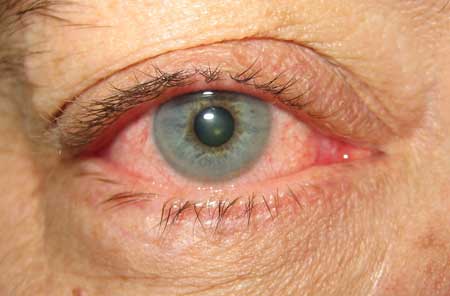
- red eye
- eyelids stuck together in morning
- tender, preauricular lymphadenopathy
Other diagnostic factors
- conjunctival follicles
- chemosis
- swollen eyelids
- superficial punctate keratopathy
- unilateral symptoms and signs
- use of medications that may lead to eye irritation
- contact lens use
- corneal subepithelial infiltrates
- corneal pannus
- vesicular skin rash
- symptoms and signs of related systemic disease
Risk factors
- exposure to infected person
- infection in one eye
- environmental irritants
- allergen exposure
- concurrent infection
- camps, swimming pools, military bases
- hot, dry climate
- atopic dermatitis
- contact lens use
- ocular prosthesis
- trauma: mechanical, chemical, or ultraviolet
- recent surgery or exposed sutures
- rosacea
- allogeneic stem cell transplantation
- Stevens-Johnson syndrome/toxic epidermal necrolysis (TEN)
- prior infection with herpes simplex virus
- in neonate: vaginal delivery
- oculogenital spread
- asthma
- hay fever
- use of topical eye medications
- use of oral antihistamine or anticholinergic drugs
- neoplasia
- history of rheumatologic disease
- dysthyroid states
- immunocompromised state
- vasculitis
- nasolacrimal duct obstruction
- abnormality of supporting structures of the eye (adnexa)
- severe tear deficiency
- trauma
- use of biologic agents
Diagnostic tests
1st tests to order
- rapid adenovirus immunoassay
Tests to consider
- cell culture
- special stains (Gram, Giemsa)
- polymerase chain reaction
- ocular pH
- allergy skin testing
- tear immunoglobulin E level
Treatment algorithm
allergic conjunctivitis (seasonal/perennial)
bacterial conjunctivitis
chlamydial conjunctivitis (inclusion)
viral conjunctivitis
neonatal conjunctivitis
contact lens related
mechanical conjunctivitis
toxic/chemical conjunctivitis
medication-related conjunctivitis
Contributors
Authors
Robert Sambursky, MD
Fellowship-Trained Ophthalmologist
Manatee Sarasota Eye Clinic & Laser Center
Bradenton
FL
Disclosures
RS is employed by Verséa Ophthalmics and serves on the board of Visus Therapeutics.
Acknowledgements
Dr Robert Sambursky would like to gratefully acknowledge Dr Lee Raykovicz, a previous contributor to this topic.
Disclosures
LR declared he was Director of Clinical Relations, Rapid Pathogen Screening, Inc.
Peer reviewers
Michael Ehrenhaus, MD
Director
Cornea, External Disease & Refractive Surgery
Long Island College Hospital Eye Center
Assistant Professor of Ophthalmology
SUNY Downstate Medical Center
Brooklyn
NY
Disclosures
ME declares that he has no competing interests.
Scott Fraser, MD, FRCS (Ed), FRCOphth
Consultant Ophthalmologist
Sunderland Eye Infirmary
Sunderland
UK
Disclosures
SF declares that he has no competing interests.
References
Key articles
Cheung, Albert Y. et al. Conjunctivitis preferred practice pattern. Ophthalmology. 2024 Feb 12;131(4): 134-204.Full text
Castillo M, Scott NW, Mustafa MZ, et al. Topical antihistamines and mast cell stabilisers for treating seasonal and perennial allergic conjunctivitis. Cochrane Database Syst Rev. 2015 Jun 1;(6):CD009566.Full text Abstract
Chen YY, Liu SH, Nurmatov U, et al. Antibiotics versus placebo for acute bacterial conjunctivitis. Cochrane Database Syst Rev. 2023 Mar 13;3(3):CD001211.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Dry eyes
- Blepharitis
- Episcleritis
More DifferentialsGuidelines
- Conjunctivitis preferred practice pattern
- Cornea/external disease summary benchmarks
More GuidelinesPatient information
Conjunctivitis
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer