Summary
Definition
History and exam
Key diagnostic factors
- pain on swallowing
- fever (>100.5°F [>38°C])
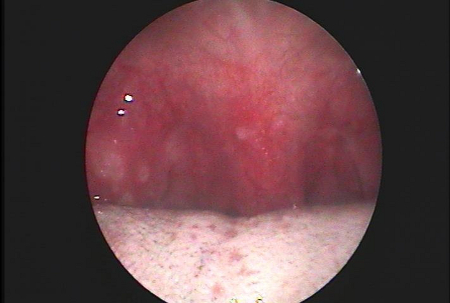
- tonsillar exudate
Other diagnostic factors
- sudden onset of sore throat
- headache
- abdominal pain
- nausea and vomiting
- presence of cough or runny nose
- tonsillar erythema
- tonsillar enlargement
- enlarged anterior cervical lymph nodes
Risk factors
- age between 5 and 15 years
- contact with infected people in enclosed spaces (e.g., child care centers, schools, prison)
Diagnostic tests
1st tests to order
- throat culture
- rapid streptococcal antigen test
Tests to consider
- serologic testing for streptococci
- WBC count and differential
- heterophile antibodies
- vaginal and cervical, or penile, and rectal cultures
- HIV viral load assay
- lateral cervical view x-ray, exposed for soft tissue
Treatment algorithm
acute tonsillitis not due to group A beta-hemolytic streptococcal infection
acute tonsillitis due to group A beta-hemolytic streptococcal infection
recurrent episodes of tonsillitis
Contributors
Authors
Christos Georgalas, PhD, DLO, FRCS (ORL-HNS)

Professor of Surgery - Head and Neck
University of Nicosia
Cyprus
Disclosures
CG declares that he has no competing interests.
Eleftherios Margaritis, PhD, MSc, MD

Otolaryngologist - Head and Neck Surgeon
Collaborator in Otolaryngology
ENT Department
Hippokration University Hospital
Athens
Greece
Disclosures
EM declares that he has no competing interests.
Peer reviewers
Itzhak Brook, MD, MSc
Professor of Pediatrics and Medicine
Georgetown University
Washington
DC
Disclosures
IB declares that he has no competing interests.
Chris Del Mar, MB BChir, FRACGP MD, MA, FAFPHM
Dean
Faculty of Health Sciences and Medicine
Bond University
Gold Coast
Queensland
Australia
Disclosures
CDM is an author of a number of references cited in this topic.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Shaikh N, Swaminathan N, Hooper EG, et al. Accuracy and precision of the signs and symptoms of streptococcal pharyngitis in children: a systematic review. J Pediatr. 2012 Mar;160(3):487-93. Abstract
Aalbers J, O'Brien KK, Chan WS, et al. Predicting streptococcal pharyngitis in adults in primary care: a systematic review of the diagnostic accuracy of symptoms and signs and validation of the Centor score. BMC Med. 2011 Jun 1;9:67.Full text Abstract
Spinks A, Glasziou PP, Del Mar CB. Antibiotics for sore throat. Cochrane Database Syst Rev. 2013;(11):CD000023.Full text Abstract
Shulman ST, Bisno AL, Clegg HW, et al. Clinical practice guideline for the diagnosis and management of group A streptococcal pharyngitis: 2012 update by the Infectious Diseases Society of America. Clin Infect Dis. 2012 Nov 15;55(10):e86-102.Full text Abstract
de Cassan S, Thompson MJ, Perera R, et al. Corticosteroids as standalone or add-on treatment for sore throat. Cochrane Database Syst Rev. 2020 May 1;5(5):CD008268.Full text Abstract
Burton MJ, Glasziou PP, Chong LY, et al. Tonsillectomy or adenotonsillectomy versus non-surgical treatment for chronic/recurrent acute tonsillitis. Cochrane Database Syst Rev. 2014 Nov 19;(11):CD001802.Full text Abstract
Windfuhr JP, Toepfner N, Steffen G, et al. Clinical practice guideline: tonsillitis II. Surgical management. Eur Arch Otorhinolaryngol. 2016 Apr;273(4):989-1009. Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Infectious mononucleosis
- Epiglottitis
- Peritonsillar abscess (quinsy)
More DifferentialsGuidelines
- Clinical practice guideline: tonsillectomy in children (update)
- A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases: 2018 update
More GuidelinesPatient information
Sore throat
Tonsillitis
More Patient informationCalculators
Sore Throat (Pharyngitis) Evaluation and Treatment Criteria (McIsaac)
More CalculatorsLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer