Summary
Definition
History and exam
Key diagnostic factors
- blurring or distortion of vision
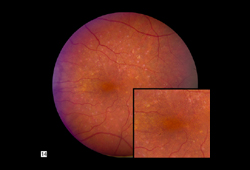
- drusen
- macular pigmentary changes
- geographic atrophy
- macular neovascularization
Other diagnostic factors
- progressive loss of vision in one or both eyes
- fibrovascular pigment epithelial detachment (neovascular age-related macular degeneration [AMD])
- fibrovascular scar formation
- subretinal drusenoid deposits
Risk factors
- increasing age
- smoking
- family history of disease
- previous cataract surgery
Diagnostic tests
1st tests to order
- Amsler grid
- optical coherence tomography
- optical coherence tomography angiography
Tests to consider
- fluorescein angiography
- indocyanine green angiography
- autofluorescence imaging
Emerging tests
- genotyping
Treatment algorithm
early stage (AREDS categories 1 and 2)
intermediate-stage (AREDS category 3)
late-stage atrophic (dry) (AREDS category 4)
late-stage exudative (wet) (AREDS category 4)
Contributors
Authors
Sajjad Mahmood, MA, MB BCHIR, FRCOphth
Consultant Ophthalmologist and Medical Retina Specialist
Honorary Clinical Lecturer
Division of Pharmacy and Optometry
Faculty of Biology, Medicine, and Health
University of Manchester
Manchester
UK
Disclosures
SM has been reimbursed by Bayer, Novartis, Roche, and Biogen for consultancy work. He has received travel grants for conference attendance and contributed to educational events for Bayer, Novartis, and Roche. He has been an investigator in industry clinical trials for Bayer, Novartis, and Roche.
Acknowledgements
Mr Sajjad Mahmood would like to gratefully acknowledge Dr Leon Charkoudian, Dr Joshua L. Dunaief, and Professor Paul Bishop, the previous contributors to this topic.
Disclosures
LC and JLD declare that they have no competing interests. PB has undertaken research activities and received research grants (from charities and the Medical Research Council) that relate to basic mechanisms underpinning age-related macular degeneration. He is an inventor on a patent for a new treatment for age-related macular degeneration filed by the University of Manchester. He does not believe that any of these activities are competing interests with respect to the content of the topic.
Peer reviewers
Sharon Fekrat, MD
Associate Professor
Vitreoretinal Surgery
Duke University Eye Center
Durham
NC
Disclosures
SF declares that she has no competing interests.
Benjamin K Young, MD, MS
Assistant Professor of Ophthalmology
Casey Eye Institute
Oregon Health & Science University
Portland
OR
Disclosures
BKY declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
American Academy of Ophthalmology. Age-related macular degeneration preferred practice pattern 2024. Feb 2025 [internet publication].Full text
National Institute for Health and Care Excellence. Age-related macular degeneration. Jan 2018 [internet publication].Full text
American Academy of Ophthalmology. Preferred practice pattern: retina summary benchmarks - 2024. Dec 2024 [internet publication].Full text
Guymer RH, Campbell TG. Age-related macular degeneration. Lancet. 2023 Apr 29;401(10386):1459-72. Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Idiopathic polypoidal choroidal vasculopathy
- Pachychoroid spectrum
- Basal laminar drusen
More DifferentialsGuidelines
- Clinical practice guide for the diagnosis and management of age-related macular degeneration
- Age related macular degeneration services: recommendations
More GuidelinesPatient information
Macular degeneration
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer