Antiparasitic monotherapy recommended as treatment option for select cases of cystic echinococcosis
The World Health Organization (WHO) has published a new evidence-based guideline on the management options available for the treatment of cystic echinococcosis. The purpose of the guideline is to provide guidance on the choice of treatment so that patients can be offered appropriate, affordable, and equitable treatment in the context of available infrastructure and expertise to ensure safety and avoid unnecessary invasive interventions.
The WHO recommends treatment according to the stage and size of cysts. Treatment with albendazole (an antiparasitic agent) monotherapy is suggested for stage CE1, CE2, CE3a, and CE3b uncomplicated hepatic cysts that are less than 5 cm in size. For larger uncomplicated hepatic cysts, percutaneous, or surgical treatment is recommended depending on the cyst type, size, and response to initial treatment. Percutaneous and surgical treatments are often combined with albendazole. Praziquantel, given in combination with albendazole, is recommended after these procedures when cyst spillage is suspected or confirmed. Due to a lack of available data, these recommendations are based on very low-certainty evidence or expert consensus.
Inactive cysts (types CE4 and CE5) are typically treated with a “watch and wait” approach. Complicated hepatic cysts and pulmonary cysts are usually managed with surgery. However, a 6-month course of albendazole monotherapy may be considered in patients with small pulmonary cysts. However, it is uncertain whether albendazole alone can effectively treat these cysts.
Cystic echinococcosis represents a substantial disease burden in rural and pastoral communities in lower- and upper-middle-income countries. It is considered a significant problem in South America, North Africa, Eastern and Mediterranean Europe, the Russian Federation, the Middle East, Central Asia, and China
Summary
Definition
History and exam
Key diagnostic factors
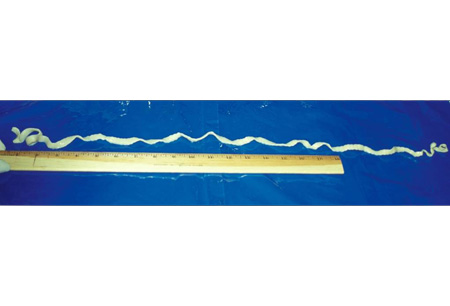
- worm segments in stool
- increased intracranial pressure
- seizures
- hepatomegaly
- cough
- hemoptysis
- chest pain
- allergy manifestations
- signs of anemia
Other diagnostic factors
- asymptomatic
- vague intestinal symptoms
- sleep disturbance
- headaches
- rash
- subcutaneous nodules
- signs of sepsis
- right upper quadrant/epigastric pain
- dyspnea
- heart palpitations
- visual disturbances
Risk factors
- living on farms
- poor hygiene
- eating or handling undercooked meat
- eating or handling undercooked fish or crustaceans
- ingestion of contaminated water
- dog owners
- outdoor pursuits
- age <12 years
Diagnostic tests
1st tests to order
- stool exam
- complete blood count
- enzyme-linked immunoelectrotransfer blot (EITB)
- echinococcus enzyme-linked immunosorbent assay (ELISA) and Western blot serology
- abdominal/thoracic ultrasound
- MRI of chest/abdomen
- echocardiogram
- CT of brain
- MRI of brain/spine
Tests to consider
- screening for tuberculosis and strongyloidiasis
Treatment algorithm
central nervous system disease: with elevated intracranial pressure
intestinal disease
central nervous system disease: without elevated intracranial pressure
hepatic or thoracic disease
Contributors
Authors
Jose A. Serpa, MD, MS, PhD
Professor of Medicine
Division of Infectious Diseases, Department of Medicine
University of Texas at Tyler
Tyler
TX
Disclosures
JAS declares that he has no competing interests.
Acknowledgements
Dr Jose A. Serpa would like to gratefully acknowledge Dr Andrew Chou, Dr Christina Coyle, and Dr Maheen Saeed, previous contributors to this topic.
Disclosures
AC and MS declare that they have no competing interests. CC is an author of several references cited in this topic.
Peer reviewers
William A. Petri, Jr, MD, PhD, FACP
Chief and Professor of Medicine
Division of Infectious Diseases and International Health
University of Virginia Health System
Charlottesville
VA
Disclosures
WAP declares that he has no competing interests.
Linda Kalilani, MBBS, MPhil, PhD
Epidemiologist
College of Medicine
University of Malawi
Zomba
Malawi
Disclosures
LK declares that she has no competing interests.
Paul Roberts, MD
Assistant Professor
Family Medicine
Mayo Clinic
Jacksonville
FL
Divulgaciones
PR declares that he has no competing interests.
Agradecimiento de los revisores por pares
Los temas de BMJ Best Practice se actualizan de forma continua de acuerdo con los desarrollos en la evidencia y en las guías. Los revisores por pares listados aquí han revisado el contenido al menos una vez durante la historia del tema.
Divulgaciones
Las afiliaciones y divulgaciones de los revisores por pares se refieren al momento de la revisión.
Referencias
Artículos principales
World Health Organization. WHO guidelines for the treatment of patients with cystic echinococcosis. Jun 2025 [internet publication].Texto completo
White AC Jr, Coyle CM, Rajshekhar V, et al. Diagnosis and treatment of neurocysticercosis: 2017 clinical practice guidelines by the Infectious Diseases Society of America (IDSA) and the American Society of Tropical Medicine and Hygiene (ASTMH). Clin Infect Dis. 2018 Apr 3;66(8):e49-75.Texto completo Resumen
World Health Organization. WHO guidelines on management of Taenia solium neurocysticercosis. Sep 2021 [internet publication].Texto completo
Del Brutto OH, Nash TE, White AC Jr, et al. Revised diagnostic criteria for neurocysticercosis. J Neurol Sci. 2017 Jan 15;372:202-10.Texto completo Resumen
Artículos de referencia
Una lista completa de las fuentes a las que se hace referencia en este tema está disponible para los usuarios con acceso a todo BMJ Best Practice.
Diferenciales
- Central nervous system tuberculoma
- Amebic abscess
- Migraine
Más DiferencialesGuías de práctica clínica
- CDC Yellow Book: health information for international travel - post-travel parasitic disease including evaluation of eosinophilia
- WHO guidelines for the treatment of patients with cystic echinococcosis
Más Guías de práctica clínicaInicie sesión o suscríbase para acceder a todo el BMJ Best Practice
El uso de este contenido está sujeto a nuestra cláusula de exención de responsabilidad