Resumen
Definición
Anamnesis y examen
Principales factores de diagnóstico
- diastolic murmur
Otros factores de diagnóstico
- dyspnea
- fatigue
- weakness
- orthopnea
- paroxysmal nocturnal dyspnea
- pallor
- mottled extremities
- rapid and faint peripheral pulse
- jugular venous distension
- basal lung crepitations
- altered mental status
- urine output <30 mL/hour
- soft S1
- soft or absent A2
- collapsing (water hammer or Corrigan) pulse
- cyanosis
- tachypnea
- displaced, hyperdynamic apical impulse
- chest pain
- pink frothy sputum
- wheeze (cardiac asthma)
- additional heart sounds
- arrhythmias
- ejection systolic flow murmur
- Austin Flint murmur
- systolic thrill
- Hill sign
- Bisferiens pulse
- de Musset sign
- Muller sign
- Traube sign
- Quincke sign
- Duroziez sign
- Mayen sign
- Lighthouse sign
- Becker sign
- Landolfi sign
- Rosenbach sign
- Gerhardt sign
- Lincoln sign
- Sherman sign
- palmar click
- syncope
Factores de riesgo
- bicuspid aortic valve
- rheumatic fever
- endocarditis
- Marfan syndrome and related connective tissue disease
- systemic hypertension
- aortitis
- older age
Pruebas diagnósticas
Primeras pruebas diagnósticas para solicitar
- ECG
- chest x-ray
- echocardiogram
- M-mode and 2-dimensional imaging
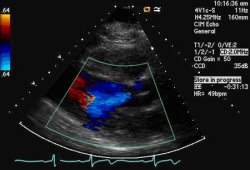
- color flow Doppler
- pulsed wave Doppler
- continuous wave Doppler
Pruebas diagnósticas que deben considerarse
- radionuclide angiography
- MRI
- exercise stress testing
- cardiac catheterization
Algoritmo de tratamiento
acute AR
chronic AR: mild to moderate
chronic AR: severe, asymptomatic
chronic AR: severe, symptomatic
Colaboradores
Autores
Poorna R. Karuparthi, MD, FACC
Associate Professor of Medicine
University of Missouri-Columbia
Chief of Cardiology
Harry S. Truman Veterans' Hospital
Columbia
MO
Divulgaciones
PRK declares that he has no competing interests.
Agradecimientos
Dr Poorna R. Karuparthi would like to gratefully acknowledge Dr Sanjeev Wasson and Dr Nishant Kalra, previous contributors to this topic.
Divulgaciones
SW and NK declare that they have no competing interests.
Revisores por pares
Kul Aggarwal, MD, MRCP, FACC, FACP
Professor of Clinical Medicine
University of Missouri-Columbia
Chief
Cardiology Section
Harry S. Truman Veterans Hospital
Columbia
MO
Divulgaciones
KA declares that he has no competing interests.
Rajdeep Khattar, DM, FRCP, FACC, FESC
Consultant Cardiologist and Honorary Senior Clinical Lecturer
Manchester Heart Centre
Central Manchester and Manchester Children's NHS Foundation Trust
Manchester
UK
Divulgaciones
RK declares that he has no competing interests.
John Pepper, MChir FRCS
Consultant Cardiac Surgeon
Department of Surgery
Royal Brompton Hospital
London
UK
Divulgaciones
JP declares that he has no competing interests.
Agradecimiento de los revisores por pares
Los temas de BMJ Best Practice se actualizan de forma continua de acuerdo con los desarrollos en la evidencia y en las guías. Los revisores por pares listados aquí han revisado el contenido al menos una vez durante la historia del tema.
Divulgaciones
Las afiliaciones y divulgaciones de los revisores por pares se refieren al momento de la revisión.
Referencias
Artículos principales
Writing Committee Members, Otto CM, Nishimura RA, et al. 2020 ACC/AHA guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2021 Feb 2;77(4):e25-197.Texto completo Resumen
Vahanian A, Beyersdorf F, Praz F, et al. 2021 ESC/EACTS guidelines for the management of valvular heart disease. Eur Heart J. 2022 Feb 12;43(7):561-632.Texto completo Resumen
Artículos de referencia
Una lista completa de las fuentes a las que se hace referencia en este tema está disponible para los usuarios con acceso a todo BMJ Best Practice.
Diferenciales
- Mitral regurgitation (MR)
- Mitral stenosis
- Aortic stenosis
Más DiferencialesGuías de práctica clínica
- 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain
- 2021 ESC/EACTS guidelines for the management of valvular heart disease
Más Guías de práctica clínicaFolletos para el paciente
Heart failure
Más Folletos para el pacienteVideos
Aortic regurgitation (severe)
Third heart sound gallop
Más vídeosInicie sesión o suscríbase para acceder a todo el BMJ Best Practice
El uso de este contenido está sujeto a nuestra cláusula de exención de responsabilidad