Summary
Definition
History and exam
Key diagnostic factors
- hematemesis
Other diagnostic factors
- light-headedness/dizziness
- postural/orthostatic hypotension
- dysphagia
- odynophagia
- pain
- melena
- hematochezia
- shock
- signs of anemia
Risk factors
- condition predisposing to retching, vomiting, and/or straining
- chronic cough
- hiatus hernia
- retching during endoscopy or other instrumentation
- significant alcohol use
- previous instrumentation
- age 30-50 years
- male sex
- use of aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs)
- hiccups
- blunt abdominal trauma
- cardiopulmonary resuscitation
Diagnostic investigations
1st investigations to order
- CBC
- BUN
- creatinine and electrolytes
- LFT
- prothrombin time (PT)/INR
- PTT
- crossmatching/blood grouping
- flexible esophagogastroduodenoscopy (EGD)
Investigations to consider
- CT chest
- CXR
- angiography
Treatment algorithm
all patients
Contributors
Expert advisers
Douglas G. Adler, MD, FACG, AGAF, FASGE
Professor of Medicine
Center Director
Center for Advanced Therapeutic Endoscopy (CATE)
Advent Health
Porter Adventist Hospital
Denver
CO
Disclosures
DGA is a consultant for Merit Medical, Cook Endoscopy, Olympus America, and Boston Scientific.
Acknowledgements
Dr Douglas Adler would like to gratefully acknowledge Dr Shilpa Reddy and Dr Juan Carlos Munoz, the previous contributors to this topic.
Disclosures
SR and JCM declare that they have no competing interests.
Peer reviewers
Joseph Sung, MD
Professor of Medicine
Department of Medicine and Therapeutics
Director
Institute of Digestive Disease
The Chinese University of Hong Kong
Hong Kong
Disclosures
JS declares that he has no competing interests.
Imtiyaz Mohammed, MD
Consultant Gastroenterologist
Sandwell General Hospital
Lyndon
West Bromwich
UK
Disclosures
IM declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Alali AA, Barkun AN. An update on the management of non-variceal upper gastrointestinal bleeding. Gastroenterol Rep (Oxf). 2023 Mar 20;11:goad011.Full text Abstract
Laine L, Barkun AN, Saltzman JR, et al. ACG clinical guideline: upper gastrointestinal and ulcer bleeding. Am J Gastroenterol. 2021 May 1;116(5):899-917.Full text Abstract
Barkun AN, Almadi M, Kuipers EJ, et al. Management of nonvariceal upper gastrointestinal bleeding: guideline recommendations from the International Consensus Group. Ann Intern Med. 2019 Dec 3;171(11):805-22.Full text Abstract
American College of Radiology. ACR appropriateness criteria: nonvariceal upper gastrointestinal bleeding. 2024 [internet publication].Full text
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Esophagitis
- Spontaneous esophageal perforation (Boerhaave syndrome)
- Cameron erosions
More DifferentialsGuidelines
- ACR appropriateness criteria: nonvariceal upper gastrointestinal bleeding
- American College of Gastroenterology - Canadian Association of Gastroenterology clinical practice guideline: management of anticoagulants and antiplatelets during acute gastrointestinal bleeding and the periendoscopic period
More GuidelinesCalculators
Blatchford score for gastrointestinal bleeding
Rockall Score for Upper Gastrointestinal Bleeding
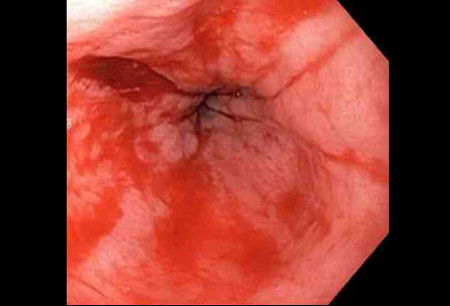
More CalculatorsVideos
Bleeding Mallory Weiss tear
Mallory Weiss tear following cauterization with a bipolar probe
More videosPatient information
Bulimia
Hernia
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer