Summary
Definition
History and exam
Key diagnostic factors
- nausea and vomiting
- abdominal distention
- no features of mechanical obstruction or peritoneal inflammation (e.g., abdominal hernia, peritoneal signs)
Other diagnostic factors
- obstipation (severe constipation with no passage of stool or flatus)
- discomfort and abdominal cramping
- decreased or hypoactive bowel sounds
- hypovolemia
Risk factors
- abdominal surgery
- acute/systemic illness (e.g., myocardial infarction, pneumonia, acute cholecystitis, pancreatitis, sepsis, multi-organ trauma)
- nonabdominal surgery
- electrolyte imbalance
- opioid analgesics, anticholinergics, or anesthetic gases
- comorbidities (e.g., diabetes mellitus, cardiovascular insufficiency, Chagas disease, scleroderma)
Diagnostic investigations
1st investigations to order
- serum electrolytes
- serum magnesium
- CBC
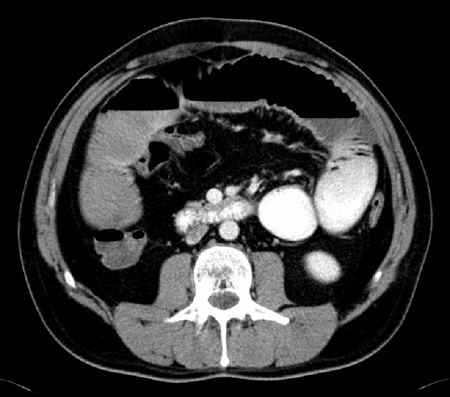
- abdomen and pelvis CT scan (with intravenous contrast and oral water soluble contrast)
Investigations to consider
- serum LFTs
- serum amylase
- serum lipase
- small bowel series
- gastric emptying study
Treatment algorithm
postoperative ileus
nonsurgical cause
ileus lasting longer than 3 days or prolonging the postoperative recovery
Contributors
Expert advisers
Steven D. Wexner, MD, PhD (Hon), FACS, FRCS (Eng), FRCS (Ed), FRCSI (Hon)
Director
Digestive Disease Center
Professor and Chair
Department of Colorectal Surgery
Cleveland Clinic
Weston
FL
Disclosures
SDW has received consulting fees, stock options, and royalties from the following companies. These relationships are ongoing. Consulting: ICON Language Services, Intuitive Surgical, Stryker, Medtronic, Takeda, ARC/Corvus, Astellas, Baxter, Olympus, AIS Channel, Livsmed. Royalties: Medtronic, Intuitive Surgical, Karl Storz Endoscopy-America, Unique Surgical Innovations. Stock Options: Regentys, LifeBond, Pragma/GibLib, and Renew Medical.
Sameh Hany Emile Rizkalla, MBBCh, MSc, MD, FACS
Research associate, Colorectal Surgery Department
Digestive Disease Center
Professor and Chair
Department of Colorectal Surgery
Cleveland Clinic
Weston
FL
Disclosures
SHER declares that he has no competing interests.
Acknowledgements
Dr Steven D. Wexner would like to gratefully acknowledge the contribution of Dr Stephen P. Sharp to the update for this topic. Dr Wexner would also like to acknowledge Dr Ahmed Sami Chadi, and Dr Paula I. Denoya, previous contributors to this topic.
Disclosures
SPS, ASC, and PID declare that they have no competing interests.
Peer reviewers
David J. Hackam, MD, PhD
Associate Professor of Pediatric Surgery
University of Pittsburgh School of Medicine
Pittsburgh
PA
Disclosures
DJH declares that he has no competing interests.
John Jenkins, MB CHB, FRCP
Consultant Colorectal Surgeon
St. Mark's Hospital
Harrow
UK
Disclosures
JJ declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Wattchow D, Heitmann P, Smolilo D, et al. Postoperative ileus- an ongoing conundrum. Neurogastroenterol Motil. 2021 May;33(5):e14046. Abstract
Gustafsson UO, Scott MJ, Hubner M, et al. Guidelines for perioperative care in elective colorectal surgery: Enhanced Recovery After Surgery (ERAS(®)) Society recommendations: 2018. World J Surg. 2019 Mar;43(3):659-95.Full text Abstract
American College of Radiology. ACR appropriateness criteria: suspected small-bowel obstruction. 2019 [internet publication].Full text
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Mechanical bowel obstruction
- Pseudo-obstruction (Ogilvie syndrome)
- Gastroenteritis
More DifferentialsGuidelines
- ACR appropriateness criteria: suspected small-bowel obstruction
- Guidelines for perioperative care in elective colorectal surgery
More GuidelinesVideos
Nasogastric tube insertion animated demonstration
More videosLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer