Tests
1st tests to order
chest x-ray
Test
Order a chest x-ray as soon as possible in all patients admitted to hospital with suspected CAP to confirm or exclude the diagnosis. In general, performing a chest x-ray in outpatients with suspected CAP is not routinely necessary.
Posteroanterior and latero-lateral projections increase the likelihood of diagnosis of pneumonia and are useful in establishing the severity of the illness. [Figure caption and citation for the preceding image starts]: Posterior-anterior chest radiograph showing right upper lobe consolidation in a patient with community-acquired pneumoniaDurrington HJ, et al. Recent changes in the management of community acquired pneumonia in adults. BMJ 2008 Jun 21;336(7658):1429-33. [Citation ends].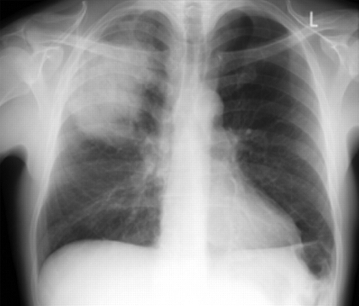
Result
new infiltrate provides definitive diagnosis of pneumonia
CBC
Test
Order in all hospitalized patients. Elevated white cell count is suggestive of infective process. Neutrophil predominance, especially if immature neutrophils, is suggestive of bacterial infection even with a normal or low white cell count. Hematocrit is used as a factor in severity scoring.
Result
leukocytosis
serum electrolytes/blood urea nitrogen
liver function tests
Test
Order in all hospitalized patients. Baseline blood should be taken. Provides information about liver function. Pneumonia is common in hospitalized patients with cirrhosis, and chronic liver disease is a risk factor for pulmonary complication in patients hospitalized due to pneumococcal pneumonia.[64]
Result
usually normal
blood glucose
Test
Order in all hospitalized patients. Baseline blood should be taken. Blood glucose levels are used in severity scoring.
Result
may be elevated
arterial blood gases/oximetry
Test
Measure in all severely ill or hospitalized patients. Indicates severity of the pneumonia.
Oximetry is noninvasive and can be used continually.
Result
may reveal low arterial oxygen saturation
blood culture
Test
Obtain pretreatment blood cultures in the following patients in the hospital setting:[18]
Patients with severe CAP as defined by American Thoracic Society (ATS)/Infectious Diseases Society of America (IDSA) criteria for defining severe CAP (see Diagnostic criteria), especially if they are intubated
Patients being empirically treated for methicillin-resistant Staphylococcus aureus (MRSA) or Pseudomonas aeruginosa
Patients who have been previously infected with MRSA or P aeruginosa, especially those with a prior respiratory tract infection
Patients who have been hospitalized and received parenteral antibiotics in the past 90 days.
Result
growth of causative bacterial species
sputum culture
Test
Obtain pretreatment Gram stain and culture of lower respiratory secretions in the following patients in the hospital setting:[18]
Patients with severe CAP as defined by American Thoracic Society (ATS)/Infectious Diseases Society of America (IDSA) criteria for defining severe CAP (see Diagnostic criteria), especially if they are intubated
Patients being empirically treated for methicillin-resistant Staphylococcus aureus (MRSA) or Pseudomonas aeruginosa
Patients who have been previously infected with MRSA or P aeruginosa, especially those with a prior respiratory tract infection
Patients who have been hospitalized and received parenteral antibiotics in the past 90 days.
Sputum Gram stain is sensitive and highly specific for identifying the causative pathogens in patients with CAP. A meta-analysis found that this test is highly specific for identifying Streptococcus pneumoniae, Haemophilus influenzae, S aureus, and gram-negative bacilli. However, the proportion of false-negative results ranged from 22% (for H influenzae) to 44% (for S pneumoniae), indicating that a negative result does not conclusively confirm the absence of causative pathogens.[79]
Result
growth/visualization of causative bacterial species
Tests to consider
point-of-care lung ultrasound
Test
Consider ordering if the chest x-ray is negative and the patient is older and frail or the clinical suspicion is uncertain.[72]
The American College of Physicians recommends point-of-care ultrasound if there is diagnostic uncertainty in patients with acute dyspnea.[73] Lung ultrasound represents an easy and accessible technique for the diagnosis of CAP. It is radiation-free, and its use is especially valuable when chest x-ray is not available. The diagnosis of CAP via bedside lung ultrasound mainly depends on detecting consolidation. However, consolidation is not always present in CAP, because pneumonia may be interstitial or present as diffuse pulmonary infiltrations.[74] Evidence shows that lung ultrasound can diagnose pneumonia in adults with excellent accuracy, including in the emergency department.[75][76][77]
Result
consolidation may be seen
CT chest
Test
Consider ordering only in patients who have an uncertain diagnosis after both a chest x-ray and ultrasound.[72]
The primacy of chest x-ray in making the diagnosis of CAP has been challenged by studies using CT scanning. Chest CT may improve the diagnosis of CAP, because chest x-ray may lead to misdiagnosis. Chest CT provides detailed information about the lung parenchyma and the mediastinum. However, the principal limitations include exposure to radiation, high cost, and the impossibility of bedside testing. One study has reported that in patients presenting to the emergency department with suspected CAP, early CT scan findings, when CT is used in addition to chest x-ray, markedly affect both diagnosis and clinical management.[78]
Result
consolidation, cavitation, effusions, neoplasm
urinary antigen testing for Legionella and pneumococcus
Test
Test urine for pneumococcal antigen in patients with severe CAP.[18]
Test urine for Legionella antigen in patients with epidemiologic factors (e.g., association with legionella outbreak or recent travel) or patients with severe CAP. Collect lower respiratory tract secretions for Legionella culture or nucleic acid amplification in patients with severe CAP at the same time.[18]
Result
positive for Legionella or pneumococcal antigens
serum C-reactive protein
Test
Consider ordering. A sensitive marker of progress in pneumonia; should be measured regularly in severely ill patients. High levels at initial presentation represent a risk factor for inadequate response to treatment, whereas low levels are protective.[82][83]
Result
may be elevated; level >10 mg/dL makes pneumonia likely
serum procalcitonin
Test
Do not order without an established, evidence-based protocol.[80] The American College of Emergency Physicians and ATS/IDSA do not recommend the routine use of procalcitonin when deciding on administration of antibiotics in the emergency department.[18][81]
Procalcitonin is a sensitive marker of progress in pneumonia. High levels at initial presentation represent a risk factor for inadequate response to treatment, whereas low levels are protective.[82] Especially elevated in cases of pneumococcal pneumonia.[84][85]
Initial empiric antibiotic therapy should be started in patients with clinically suspected and radiographically confirmed CAP regardless of the initial serum procalcitonin level.[18]
Result
may be elevated
thoracocentesis and pleural fluid culture
Test
Consider ordering in all patients with a pleural effusion. Positive Gram stain of pleural fluid indicates an empyema.
Result
exudate; growth of causative bacterial species in case of empyema
bronchoscopy
Test
Consider ordering in immunosuppressed patients, in patients with severe CAP, and in cases of treatment failure.
The most common techniques are bronchoalveolar lavage (BAL) and protected specimen brushing (PSB).
Result
BAL: 10⁴ colony-forming units (CFU)/mL indicates infection; PSB: 10³ CFU/mL has been recommended to distinguish colonization from infection
tests for respiratory viruses
Test
Test for influenza virus using a rapid influenza molecular assay (rather than antigen-based detection tests) when influenza viruses are circulating in the community. Testing may also be considered during periods of low influenza activity.[18]
Rapid antigen testing or direct fluorescent antibody testing can be used to detect other respiratory viruses and can help with decisions regarding antiviral therapy and may reduce the use of antibacterial agents. Do not order broad respiratory pathogen panels unless the result will directly influence management decisions.[80]
Result
detection of viral antigens or antibodies
molecular microbiological techniques
Test
Includes polymerase chain reaction. Used for bacteria (including atypical pathogens) and respiratory viruses. These tests are rapid and the results may help to guide antimicrobial therapy. Also, new techniques offer antimicrobial resistance patterns and quantified bacteria loads, which may be linked to the degree of infection, as has been shown particularly in pneumococcal infection. The American Thoracic Society recommends nucleic acid-based testing of respiratory samples for viral pathogens other than influenza only in hospitalized patients with suspected CAP who either have severe CAP or are immunocompromised. Routine use of nucleic acid-based testing is not recommended in outpatients with suspected CAP.[88]
Result
detection of pathogenic organism
Use of this content is subject to our disclaimer
