Summary
Definition
History and exam
Key diagnostic factors
- visual disturbance in one eye
- peculiar sensory phenomena
Other diagnostic factors
- female sex
- age 20-40 years
- foot dragging or slapping
- leg cramping
- fatigue
- urinary frequency
- bowel dysfunction
- spasticity/increased muscle tone
- increased deep tendon reflexes
- imbalance/incoordination
- pale optic disk or noncorrectable visual loss
- incorrect responses to Ishihara color blindness test plates
- abnormal eye movements
Risk factors
- female sex
- family history of MS
- northern latitude
- genetic factors
- smoking
- vitamin D deficiency
- autoimmune disease
- Epstein-Barr virus
- overweight/obesity in children and adolescents
Diagnostic tests
1st tests to order
- MRI - brain
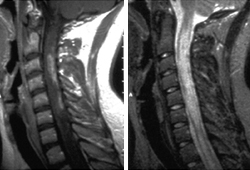
- MRI - spinal cord
- CBC
- comprehensive metabolic panel
- thyroid-stimulating hormone
- vitamin B12
Tests to consider
- antibody testing for neuromyelitis optica spectrum disorders (NMOSD)
- cerebrospinal fluid evaluation
- evoked potentials
Treatment algorithm
acute relapse affecting function
relapsing-remitting MS
secondary progressive MS
primary progressive MS
Contributors
Authors
Mary Alissa Willis, MD
Associate Professor and Chair
Department of Neurology
University of Mississippi Medical Center
Jackson
MS
Disclosures
MAW has been compensated for Speakers' Bureau participation with Alexion, Biogen, Bristol-Myers Squibb, Genzyme, and Genentech, and advisory board participation with Alexion, Biogen, Greenwich Biosciences, Genentech, and Horizon.
Acknowledgements
Dr Mary Alissa Willis would like to gratefully acknowledge Dr Lael A. Stone, a previous contributor to this topic. We have since been made aware that Dr Stone is deceased.
Peer reviewers
Alex Rae-Grant, MD
Project Leader for Neurology
Neurological Institute
Cleveland Clinic
Cleveland
OH
Disclosures
ARG declares that he has no competing interests.
Sarah A. Morrow, MD, FRCPC, MS
Associate Professor of Neurology
Department of Clinical Neurological Sciences
London Health Sciences Centre
University Hospital
Ontario
Canada
Disclosures
SAM declares that she has no competing interests.
Marcelo Kremenchutzky, MD
Director
The London Multiple Sclerosis Clinic
Associate Professor
Schulich School of Medicine
University of Western Ontario
Neurologist
Clinical Neurological Sciences Department
University Hospital
London Health Sciences Centre
Ontario
Canada
Disclosures
MK declares that he has no competing interests.
Abhijit Chaudhuri, DM, MD, PhD, FACP, FRCPGlasg, FRCPLond
Consultant Neurologist
Department of Neurology
Queen’s Hospital
Romford
UK
Disclosures
AC declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Wattjes MP, Ciccarelli O, Reich DS, et al. 2021 MAGNIMS-CMSC-NAIMS consensus recommendations on the use of MRI in patients with multiple sclerosis. Lancet Neurol. 2021 Aug;20(8):653-670.Full text Abstract
Thompson AJ, Banwell BL, Barkhof F, et al. Diagnosis of multiple sclerosis: 2017 revisions of the McDonald criteria. Lancet Neurol. 2018 Feb;17(2):162-73. Abstract
Montalban X, Gold R, Thompson AJ, et al. ECTRIMS/EAN guideline on the pharmacological treatment of people with multiple sclerosis. Mult Scler. 2018 Feb;24(2):96-120.Full text Abstract
Rae-Grant A, Day GS, Marrie RA, et al. Practice guideline recommendations summary: disease-modifying therapies for adults with multiple sclerosis. Neurology. 2018 Apr 24;90(17):777-88.Full text Abstract
Solari A, Giordano A, Sastre-Garriga J, et al. EAN guideline on palliative care of people with severe, progressive multiple sclerosis. Eur J Neurol. 2020 Aug;27(8):1510-29.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Myelopathy due to cervical spondylosis
- Fibromyalgia
- Postural orthostatic tachycardia syndrome with or without cervicogenic migraine
More DifferentialsGuidelines
- Clinical guidance in neuropalliative care: an AAN position statement
- Multiple sclerosis in adults: management
More GuidelinesPatient information
Multiple sclerosis
Multiple sclerosis: questions to ask your doctor
More Patient informationVideos
Diagnostic lumbar puncture in adults: animated demonstration
Venepuncture and phlebotomy: animated demonstration
More videosLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer