Summary
Definition
History and exam
Key diagnostic factors
- flu-like illness with low-grade fever, fatigue, and arthralgia
Other diagnostic factors
- cough
- shortness of breath
- bilateral crackles
Risk factors
- infectious pneumonia
- connective tissue diseases
- immunologic diseases and inflammatory bowel disease
- organ transplantation
- medication use
- breast radiation therapy
- exposure to toxins
- vaping
Diagnostic tests
1st tests to order
- chest x-ray
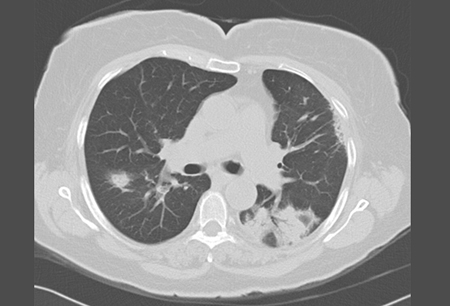
- high-resolution chest CT scan (HRCT)
- CBC
- erythrocyte sedimentation rate
Tests to consider
- CRP
- sputum culture
- atypical viral screen
- pulmonary function tests
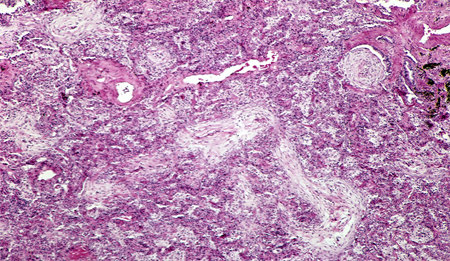
- surgical lung biopsy
- creatine kinase
- general autoimmune and myositis profile
- positron emission tomography (PET) scan
- bronchoscopy
Treatment algorithm
rapidly progressive OP
cryptogenic OP
secondary OP
recurrent OP, rapidly progressive
recurrent OP, not rapidly progressive
Contributors
Authors
O'Neil Green, MBBS, FCCP
Assistant Professor in Medicine
Director, NTM and Bronchiectasis Clinic
UMass Chan School of Medicine/Baystate Health
Worcester
MA
Disclosures
OG has been a consultant to Pharming Inc. and has received research grants from Fisher & Paykel Inc. and Insmed Inc.
Jean-Pierre Assaker, MD
Pulmonary and Critical Care Fellow
UMass Chan School of Medicine/Baystate Health
Worcester
MA
Disclosures
JA declares that he has no competing interests.
Acknowledgements
Dr O’Neil Green and Dr Jean-Pierre Assaker would like to gratefully acknowledge Dr Gary R. Epler, the previous contributor to this topic.
Disclosures
GRE is an author of several references cited in this topic.
Peer reviewers
Nazia Chaudhuri, MbChB, BSc, PhD, FRCP
Clinical Lead of ILD Service
Manchester University NHS Foundation Trust
Manchester
UK
Disclosures
NC declares that she has no competing interests.
Steven Sahn, MD
Professor of Medicine and Director
Division of Pulmonary/Critical Care/Allergy/Sleep Medicine
Medical University of South Carolina
Charleston
SC
Disclosures
SS declares that he has no competing interests.
Teofilo Lee-Chiong, MD
National Jewish Medical and Research Center
Denver
CO
Disclosures
TLC has been reimbursed by the American College of Chest Physicians (ACCP), American Academy of Sleep Medicine, American Thoracic Society, and Cephalon, the manufacturer of modafinil, for attending several conferences. He has been paid by the ACCP for running educational programs and by Elsevier for serving as consultant of the Sleep Medicine Clinics. He has also received research funding from the National Institutes of Health, Respironics, Restore, and Schwarz Pharma, and has been a member of the speakers' bureau for GlaxoSmithKline.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Epler GR, Colby TV, McLoud TC, et al. Bronchiolitis obliterans organizing pneumonia. N Engl J Med. 1985 Jan 17;312(3):152-8. Abstract
Epler GR. Bronchiolitis obliterans organizing pneumonia, 25 years: a variety of causes, but what are the treatment options? Expert Rev Respir Med. 2011 Jun;5(3):353-61. Abstract
Bradley B, Branley HM, Egan JJ, et al; British Thoracic Society Interstitial Lung Disease Guideline Group, British Thoracic Society Standards of Care Committee; Thoracic Society of Australia; New Zealand Thoracic Society; Irish Thoracic Society. Interstitial lung disease guideline. Thorax. 2008 Sep;63 Suppl 5:v1-58.Full text Abstract
Travis WD, Costabel U, Hansell DM, et al. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am J Respir Crit Care Med. 2013 Sep 15;188(6):733-48.Full text Abstract
Lazor R, Vandevenne A, Pelletier A, et al. Cryptogenic organizing pneumonia: characteristics of relapses in a series of 48 patients. Am J Respir Crit Care Med. 2000 Aug;162(2 Pt 1):571-7.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Nodular sarcoidosis
- Chronic eosinophilic pneumonia (CEP)
- Nonspecific interstitial pneumonia (NSIP)
More DifferentialsGuidelines
- ACR appropriateness criteria: chronic dyspnea-noncardiovascular origin
- An official American Thoracic Society/European Respiratory Society statement: update of the international multidisciplinary classification of the idiopathic interstitial pneumonias
More GuidelinesPatient information
Pneumonia
More Patient informationVideos
Late inspiratory crackles (rales)
More videosLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer