Summary
Definition
History and exam
Key diagnostic factors
- high fluid intake
- fluid losses
- history of diabetes mellitus
- history of cirrhosis, nephrosis, congestive heart failure
- nausea/vomiting
- mild cognitive symptoms
- altered mental status, seizures, coma
- low urine output
- weight changes
- orthostatic hypotension
- abnormal jugular venous pressure
- poor skin turgor
- dry mucus membranes
- absence of axillary sweat
- edema
- rales or crackles on lung auscultation
- polyuria
Other diagnostic factors
- history of hyperlipidemia or paraproteinemia
Risk factors
- older age
- hospitalization
- selective serotonin-reuptake inhibitor (SSRI) use
- thiazide diuretic use
- underlying medical conditions
- severe hypothyroidism
- adrenal insufficiency
- malignancy
- use of other medications
- MDMA (ecstasy) use
Diagnostic investigations
1st investigations to order
- serum sodium concentration
- serum electrolytes, BUN, creatinine, and glucose
- serum osmolality
- urine sodium concentration
- urine osmolality
- urine electrolytes
- urine flow rate
- electrolyte-free water excretion
- fractional excretion of sodium
- thyroid-stimulating hormone
- serum cortisol level and/or adrenocorticotropic hormone test
- serum lipids and serum protein electrophoresis
Investigations to consider
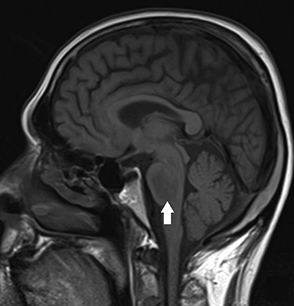
- CT brain, chest, abdomen/pelvis
- other tests targeted at evaluating the underlying cause
Treatment algorithm
acute onset (<48 hours) and/or symptomatic
chronic onset (≥48 hours) or asymptomatic
overcorrection of serum sodium concentration
Contributors
Authors
Judith H. Veis, MD

Section Director
Nephrology
MedStar Washington Hospital Center
Washington
DC
Disclosures
JHV declares that she has no competing interests.
Peer reviewers
Gregor Lindner, MD
Director
Department of Internal & Emergency Medicine
Hirslanden Klinik Im Park
Zurich
Switzerland
Disclosures
GL is an author of a number of references cited in this topic.
Michael E. Ullian, MD
Professor of Medicine
Division of Nephrology
Department of Medicine
Medical University of South Carolina
Charleston
SC
Disclosures
MEU declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Spasovski G, Vanholder R, Allolio B, et al; Hyponatraemia Guideline Development Group. Clinical practice guideline on diagnosis and treatment of hyponatraemia. Eur J Endocrinol. 2014 Feb 25;170(3):G1-47.Full text Abstract
Adrogué HJ, Tucker BM, Madias NE. Diagnosis and management of hyponatremia: a review. JAMA. 2022 Jul 19;328(3):280-91. Abstract
Verbalis JG, Grossman A, Höybye C, et al. Review and analysis of differing regulatory indications and expert panel guidelines for the treatment of hyponatremia. Curr Med Res Opin. 2014 Jul;30(7):1201-7. Abstract
Hoorn EJ, Zietse R. Diagnosis and treatment of hyponatremia: compilation of the guidelines. J Am Soc Nephrol. 2017 May;28(5):1340-9.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Hypertonic hyponatremia
- Pseudohyponatremia
- Evaluation of hyponatremia
More DifferentialsGuidelines
- Clinical practice guidelines for the management of exercise-associated hyponatremia: 2019 update
- Clinical practice guidelines for the management of exercise-associated hyponatremia: 2019 update
More GuidelinesPatient information
Hyponatremia (low blood sodium)
More Patient informationCalculators
Sodium Correction in Hyperglycemia (Hillier 1999)
Osmolality Estimator (serum)
More CalculatorsLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer