Summary
Differentials
Common
- Nonhemorrhagic volume losses
- Upper gastrointestinal bleed
- Lower gastrointestinal bleed
- Dialysis-induced hypotension
- Trauma
- Acute coronary syndrome
- Acute heart failure
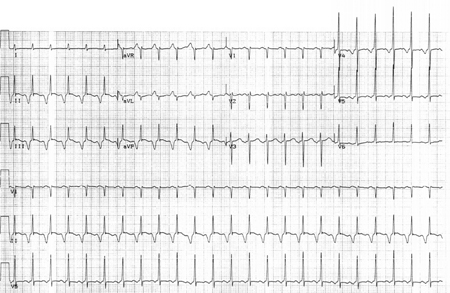
- Dysrhythmia
- Acute pulmonary embolism
- Medication-related
- Pregnancy (uncomplicated)
- Vasovagal syncope
- Sepsis
- Chronic liver disease
- Parkinson disease
Uncommon
- Ruptured abdominal aortic aneurysm (AAA)
- Ectopic pregnancy
- Retroperitoneal bleed
- Carotid sinus hypersensitivity syndrome
- Severe hypothyroidism
- Tension pneumothorax
- Cardiac tamponade
- Situational syncope
- Anaphylaxis
- Severe acute pancreatitis
- Diabetic autonomic neuropathy
- Multi-system atrophy
- Post-stroke
- Primary autonomic failure
- Amyloidosis
- Adrenal suppression (iatrogenic)
- Addison disease
- Hypopituitarism
- Thiamine deficiency
- Vitamin B12 deficiency
- Carcinoid syndrome
Contributors
Authors
Fiona Kearney, MB, BCh, BAO, MRCPI
Consultant Geriatrician
Department of Healthcare of Older People
Nottingham University Hospitals NHS Trust
Queen’s Medical Centre
Nottingham
UK
Disclosures
FK is an author of a reference cited in this topic.
Alan Moore, MB, BCh, BAO, FRCPI
Consultant Geriatrician
Beaumont Hospital
Dublin
Honorary Senior Lecturer at Royal College of Surgeons
Ireland Medical School
Dublin
Republic of Ireland
Disclosures
AM is an author of a number of references cited in this topic.
Peer reviewers
Vidhu S. Paliwal, MD
Cardiologist
Skagit Valley Hospital
Mount Vernon
WA
Disclosures
VSP declares that he has no competing interests.
Gideon Caplan, MB, BS Syd, FRACP
Director
Geriatric Medicine
Prince of Wales Hospital
Sydney
Australia
Disclosures
GC declares that he has no competing interests.
Vasi Naganathan, MBBS, FRACP, MMed (Clin Epi), PhD, Grad Cert Med Ed
Academic Sydney Medical School
University of Sydney
Consultant Geriatrician
Concord Hospital Centre for Education and Research on Ageing
Concord
Australia
Disclosures
VN declares that he has no competing interests.
Andrew Parfitt, MBBS, FFAEM
Clinical Director
Acute Medicine
Associate Medical Director
Consultant Emergency Medicine
Guy's and St Thomas' NHS Foundation Trust
Clinical Lead and Consultant
Accident Emergency Medicine
St Thomas' Hospital
London
UK
Disclosures
AP declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Brignole M, Moya A, de Lange FJ, et al. 2018 ESC guidelines for the diagnosis and management of syncope. Eur Heart J. 2018 Jun 1;39(21):1883-948.Full text
McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.Full text
Society of Critical Care Medicine; European Society of Intensive Care Medicine. Surviving Sepsis Campaign: hour-1 bundle: initial resuscitation for sepsis and septic shock. 2019 [internet publication].Full text
Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. Circulation. 2022 May 3;145(18):e895-1032.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Patient information
Sepsis in adults
Pulmonary embolism: what is it?
More Patient informationVideos
Needle decompression of tension pneumothorax: animated demonstration
Central venous catheter insertion: animated demonstration
More videosLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer