Summary
Definition
History and exam
Key diagnostic factors
- abrupt onset of high fever
- flu-like illness
- severe headache
- cough
- inspiratory crackles, rhonchi, or wheezing
- hepatomegaly
Other diagnostic factors
- exanthemas
- pleuritic chest pain
- seizures
- coma
- chronic fatigue
- signs of endocarditis or vascular infection (persistent focalized infection)
- other signs of persistent focalized infection
- other signs of acute infection
Risk factors
- exposure to infected animals
- occupational exposure
- travel or residency in endemic areas
- male sex
- age 30 to 70 years
- immunosuppression
- preexisting cardiac disease
- preexisting vasculopathy
- pregnancy
Diagnostic investigations
1st investigations to order
- indirect immunofluorescence assay (IFA)
- polymerase chain reaction (PCR)
- CBC
- CRP
- LFTs
- activated partial thromboplastin time (aPTT)
- IgG anticardiolipin (aCL) antibodies
Investigations to consider
- cerebrospinal fluid cell count and differential
- cerebrospinal fluid protein
- cerebrospinal fluid glucose
- CXR
- transthoracic echocardiography (TTE)
- transesophageal echocardiography (TEE)
- liver ultrasound
- abdominal CT scan or ultrasound
- chest CT
- brain CT
- 18F-fluorodeoxyglucose (FDG) PET/CT imaging
- lymph node biopsy
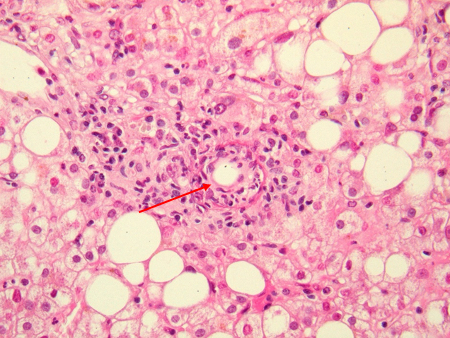
- immunohistochemistry
- fluorescence in situ hybridization (FISH)
Treatment algorithm
acute infection, nonpregnant, no severe immunodeficiency: at low risk of persistent focalized infection
acute infection, nonpregnant, no severe immunodeficiency: at high risk of persistent focalized infection
acute infection, nonpregnant, with severe immunodeficiency
acute infection, pregnant
suspected or confirmed persistent focalized infection, with no severe immunodeficiency
suspected or confirmed persistent focalized infection, with severe immunodeficiency
Contributors
Authors
Stephen Gluckman, MD
Professor of Medicine
Medical Director, Penn Global Medicine
Hospital of the University of Pennsylvania
Penn International Medicine and Immunization Clinic; Penn Center for Primary Care
Philadelphia
PA
利益声明
SG declares that he has no competing interests.
鸣谢
Professor Stephen Gluckman would like to gratefully acknowledge Dr Joshua Hartzell, Dr Matthieu Million, Professor Didier Raoult, and Dr Nilmarie Guzman, previous contributors to this topic.
利益声明
MM and DR are authors of several references cited in this topic. JH and NG declare that they have no competing interests.
同行评议者
Ron Behrens, MD, FRCP
Consultant in Tropical and Travel Medicine
Hospitals for Tropical Diseases
Senior Lecturer
London School of Hygiene and Tropical Medicine
London
UK
利益声明
RB has provided expert testimony on behalf of the Crown, to the courts in the UK, on Q fever.
Jennifer McQuiston, DVM, MS, DACVPM
Epidemiology Team
Rickettsial Zoonoses Branch
National Center for Zoonotic Vectorborne and Enteric Diseases
Centers for Disease Control and Prevention
Atlanta
GA
利益声明
JM declares that she has no competing interests.
Dimitrios Chatzidimitriou, MD, PhD
Clinical Microbiologist
National Influenza Center
Second Department of Microbiology
Aristotle University of Thessaloniki Medical School
Thessaloniki
Greece
利益声明
DC declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
参考文献
关键文献
Anderson A, Bijlmer H, Fournier PE, et al. Diagnosis and management of Q fever - United States, 2013: recommendations from CDC and the Q fever working group. MMWR Recomm Rep. 2013 Mar 29;62(RR-03):1-23.全文 摘要
National Association of State Public Health Veterinarians, National Assembly of State Animal Health Officials. Prevention and control of coxiella burnetii infection among humans and animals: guidance for a coordinated public health and animal health response, 2013. 2013 [internet publication].全文
参考文献
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
鉴别诊断
- Legionella infection
- Tularemia
- Viral hepatitis
更多 鉴别诊断指南
- Clinical guidance for Q fever
- A guide to utilization of the microbiology laboratory for diagnosis of infectious diseases
更多 指南患者教育信息
Flu
更多 患者教育信息登录或订阅即可浏览 BMJ Best Practice 临床实践完整内容
内容使用需遵循免责声明