Summary
Details
- Cervical sampling techniques
- Cervical cytology
- HPV testing
- HPV vaccination
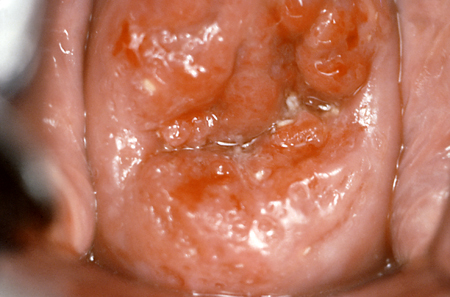
- Colposcopy
- Guidelines
Contributors
Authors
Richard T. Penson, MD, MRCP

Medical Gynecologic Oncology
Division of Hematology Oncology
Massachusetts General Hospital
Boston
MA
Disclosures
RTP reports personal fees for advisory boards from Aadi Bioscience, AstraZeneca, GSK Inc., ImmunoGen Inc., Merck & Co., Mersana, Novacure, Roche Pharma, Sutro Biopharma, and Vascular Biogenics Ltd; serves on Drug Safety and Monitoring Boards for AstraZeneca, EQRx, and Roche Pharma; Institutional research funding (as Principal Investigator) for Array BioPharma Inc., AstraZeneca., Eisai Inc., Genentech, Inc., Vascular Biogenics Ltd; and royalties from BMJ Publishing, UptoDate, Elsevier Ltd., Wolters Kluwer Health, and Wiley Blackwell. Payment for educational events: Research to Practice, ExpertConnect, ReachMD, CMEO Outfitters.
Marcela G. del Carmen, MD, MPH

President
Massachusetts General Physicians Organization
Division of Gynecologic-Oncology
Massachusetts General Hospital
Professor
Department of Obstetrics, Gynecology and Reproductive Biology
Harvard Medical School
Boston
MA
Disclosures
MDC declares that she has no competing interests.
Peer reviewers
Diane M. Harper, MD, MPH, MS
Professor
Departments of Family Medicine and Obstetrics and Gynecology
University of Michigan
Ann Arbor
MI
Disclosures
DMH has been paid through a grant from Roche to the University of Michigan.
Deirdre Lyons, MB, BCh, BAO, MRCOG
Consultant in Obstetrics & Gynaecology
Lead Clinician in Colposcopy
Imperial College Healthcare NHS Trust
London
UK
Disclosures
DL declares that she has no competing interests.
Matejka Rebolj, PhD
Scientific Researcher
Centre for Epidemiology and Screening
Institute of Public Health
University of Copenhagen
Copenhagen
Denmark
Disclosures
MR declares that she has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Fontham ETH, Wolf AMD, Church TR, et al. Cervical cancer screening for individuals at average risk: 2020 guideline update from the American Cancer Society. CA Cancer J Clin. 2020 Sep;70(5):321-46.Full text Abstract
Sawaya GF, Kulasingam S, Denberg TD, et al. Cervical cancer screening in average-risk women: best practice advice from the clinical guidelines committee of the American College of Physicians. Ann Intern Med. 2015;162:851-9.Full text Abstract
US Preventive Services Task Force., Curry SJ, Krist AH, et al. Screening for cervical cancer: US Preventive Services Task Force recommendation statement. JAMA. 2018 Aug 21;320(7):674-86.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Use of this content is subject to our disclaimer