Hypertension is a common disorder that affects a large proportion of the community. It is usually asymptomatic and is detected on routine exam or after the occurrence of a complication such as heart attack or stroke.[1]Lip GY. Hypertension, platelets, and the endothelium: the "thrombotic paradox" of hypertension (or "Birmingham paradox") revisited. Hypertension. 2003 Feb;41(2):199-200.
http://hyper.ahajournals.org/cgi/content/full/41/2/199
http://www.ncbi.nlm.nih.gov/pubmed/12574081?tool=bestpractice.com
The 2025 American Heart Association (AHA) and American College of Cardiology (ACC) guidelines for the prevention, detection, evaluation, and management of high blood pressure in adults defines hypertension as any systolic blood pressure measurement of ≥130 mmHg or any diastolic blood pressure measurement of ≥80 mmHg.[2]Jones DW, Ferdinand KC, Taler SJ, et al. 2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J Am Coll Cardiol. 2025 Nov 4;86(18):1567-678.
https://www.jacc.org/doi/10.1016/j.jacc.2025.05.007
http://www.ncbi.nlm.nih.gov/pubmed/40815242?tool=bestpractice.com
AHA/ACC blood pressure categories are defined as follows:
Elevated blood pressure: systolic blood pressure of 120-129 mmHg and diastolic blood pressure of <80 mmHg
Stage 1 hypertension: systolic blood pressure of 130-139 mmHg or diastolic blood pressure of 80-89 mmHg
Stage 2 hypertension: systolic blood pressure of ≥140 mmHg or diastolic blood pressure of ≥90 mmHg
The AHA/ACC guidelines were mainly based on the results of the SPRINT trial, which investigated intensive or standard hypertension treatment in people with a systolic blood pressure of ≥130 mmHg with an increased cardiovascular risk (but without diabetes).[3]SPRINT Research Group; Wright JT Jr, Williamson JD, Whelton PK, et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015 Nov 26;373(22):2103-16.
https://www.nejm.org/doi/10.1056/NEJMoa1511939
http://www.ncbi.nlm.nih.gov/pubmed/26551272?tool=bestpractice.com
European guideline blood pressure categories are defined as follows:[4]McEvoy JW, McCarthy CP, Bruno RM, et al. 2024 ESC guidelines for the management of elevated blood pressure and hypertension. Eur Heart J. 2024 Oct 7;45(38):3912-4018.
https://academic.oup.com/eurheartj/article/45/38/3912/7741010
Elevated blood pressure: office systolic blood pressure 120-139 mmHg or office diastolic blood pressure 70-89 mmHg
Hypertension: office systolic blood pressure ≥140 mmHg or office diastolic blood pressure ≥90 mmHg.
For the diagnosis of elevated blood pressure or hypertension to be made, the European guidelines recommend confirmation with out-of-office measurements or at least one repeat office measurement at a subsequent visit.[4]McEvoy JW, McCarthy CP, Bruno RM, et al. 2024 ESC guidelines for the management of elevated blood pressure and hypertension. Eur Heart J. 2024 Oct 7;45(38):3912-4018.
https://academic.oup.com/eurheartj/article/45/38/3912/7741010
Isolated systolic hypertension is defined as a systolic blood pressure ≥140 mmHg, with a diastolic blood pressure <90 mmHg.[4]McEvoy JW, McCarthy CP, Bruno RM, et al. 2024 ESC guidelines for the management of elevated blood pressure and hypertension. Eur Heart J. 2024 Oct 7;45(38):3912-4018.
https://academic.oup.com/eurheartj/article/45/38/3912/7741010
The UK National Institute for Health and Care Excellence states that a diagnosis of hypertension is confirmed in those with:[5]National Institute for Health and Care Excellence. Hypertension in adults: diagnosis and management. Nov 2023 [internet publication].
https://www.nice.org.uk/guidance/ng136
a clinic blood pressure of ≥140/90 mmHg, and
daytime ambulatory blood pressure monitoring average or home blood pressure monitoring average of ≥135/85 mmHg.
Although different studies have used a variety of cut-off points for the diagnosis of hypertension in the community, any blood pressure >120 mmHg systolic is associated with an increased cardiovascular risk. The importance of hypertension is its relation to other cardiovascular risk factors and consequent overall cardiovascular risk.
The AHA/ACC defines resistant hypertension as:[2]Jones DW, Ferdinand KC, Taler SJ, et al. 2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J Am Coll Cardiol. 2025 Nov 4;86(18):1567-678.
https://www.jacc.org/doi/10.1016/j.jacc.2025.05.007
http://www.ncbi.nlm.nih.gov/pubmed/40815242?tool=bestpractice.com
Blood pressure above goal (i.e., >130/80 mmHg) despite the concurrent use of at least 3 antihypertensive agents with complementary mechanisms of action (including a diuretic) at maximum or maximally tolerated doses.
Blood pressure at goal but requiring 4 or more antihypertensive agents.
The diagnosis of resistant hypertension requires the exclusion of white-coat hypertension and poor adherence with antihypertensive medication.[2]Jones DW, Ferdinand KC, Taler SJ, et al. 2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J Am Coll Cardiol. 2025 Nov 4;86(18):1567-678.
https://www.jacc.org/doi/10.1016/j.jacc.2025.05.007
http://www.ncbi.nlm.nih.gov/pubmed/40815242?tool=bestpractice.com
This topic addresses the evaluation of hypertension in adults.
Epidemiology
According to a global analysis of trends in hypertension, the number of adults ages 30-79 years with hypertension increased from 650 million to 1.28 billion in the period 1990-2019.[6]NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: a pooled analysis of 1201 population-representative studies with 104 million participants. Lancet. 2021 Sep 11;398(10304):957-80.
https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(21)01330-1/fulltext
http://www.ncbi.nlm.nih.gov/pubmed/34450083?tool=bestpractice.com
Based on National Health and Nutrition Survey (NHANES) data from 2017-2020, an estimated 122.4 million US adults ages ≥20 years have hypertension (defined as self-reported use of antihypertensive medication, systolic BP ≥130 mmHg or diastolic BP ≥80 mmHg).[7]Martin SS, Aday AW, Allen NB, et al. 2025 heart disease and stroke statistics: a report of US and global data from the American Heart Association. Circulation. 2025 Feb 25;151(8):e41-660.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001303
http://www.ncbi.nlm.nih.gov/pubmed/39866113?tool=bestpractice.com
During this period, the prevalence of hypertension was 28.5% among those ages 20-44 years, 58.6% among those ages 45-64 years, and 76.5% among those age ≥65 years.[7]Martin SS, Aday AW, Allen NB, et al. 2025 heart disease and stroke statistics: a report of US and global data from the American Heart Association. Circulation. 2025 Feb 25;151(8):e41-660.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001303
http://www.ncbi.nlm.nih.gov/pubmed/39866113?tool=bestpractice.com
The prevalence may be similar or higher in Western Europe.[8]Falaschetti E, Mindell J, Knott C, et al. Hypertension management in England: a serial cross-sectional study from 1994 to 2011. Lancet. 2014 May 31;383(9932):1912-9.
http://www.ncbi.nlm.nih.gov/pubmed/24881995?tool=bestpractice.com
[9]Lacruz ME, Kluttig A, Hartwig S, et al. Prevalence and incidence of hypertension in the general adult population: results of the CARLA-cohort study. Medicine (Baltimore). 2015 Jun;94(22):e952.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4616348
http://www.ncbi.nlm.nih.gov/pubmed/26039136?tool=bestpractice.com
In 2010, the estimated global age-standardized prevalence of hypertension in adults age ≥20 years was 31.1%; 28.5% in high-income countries and 31.5% in low- and middle-income countries.[10]Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016 Aug 9;134(6):441-50.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4979614
http://www.ncbi.nlm.nih.gov/pubmed/27502908?tool=bestpractice.com
Prevalence by sex has been found to differ with age with prevalence higher in men than in women age <65 years, but higher in women than in men age ≥65 years.[7]Martin SS, Aday AW, Allen NB, et al. 2025 heart disease and stroke statistics: a report of US and global data from the American Heart Association. Circulation. 2025 Feb 25;151(8):e41-660.
https://www.ahajournals.org/doi/10.1161/CIR.0000000000001303
http://www.ncbi.nlm.nih.gov/pubmed/39866113?tool=bestpractice.com
[10]Mills KT, Bundy JD, Kelly TN, et al. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation. 2016 Aug 9;134(6):441-50.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4979614
http://www.ncbi.nlm.nih.gov/pubmed/27502908?tool=bestpractice.com
Hypertension is more prevalent in black people than in white people, starting in childhood, with 76% of black men and women developing hypertension by age 55 years, compared with 55% and 40% of white men and women, respectively.[11]Thomas SJ, Booth JN 3rd, Dai C, et al. Cumulative incidence of hypertension by 55 years of age in blacks and whites: the CARDIA study. J Am Heart Assoc. 2018 Jul 11;7(14).
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6064834
http://www.ncbi.nlm.nih.gov/pubmed/29997132?tool=bestpractice.com
The exact prevalence of hypertension is difficult to assess, as it is usually asymptomatic. Prevalence is expected to rise as the "cut-off" value for hypertension is redefined at a lower level.
Approximately 8.5% to 20% of US adults with hypertension have resistant hypertension.[2]Jones DW, Ferdinand KC, Taler SJ, et al. 2025 AHA/ACC/AANP/AAPA/ABC/ACCP/ACPM/AGS/AMA/ASPC/NMA/PCNA/SGIM guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. J Am Coll Cardiol. 2025 Nov 4;86(18):1567-678.
https://www.jacc.org/doi/10.1016/j.jacc.2025.05.007
http://www.ncbi.nlm.nih.gov/pubmed/40815242?tool=bestpractice.com
Complications and hypertension-mediated organ damage
Studies have shown that treatment of hypertension can reduce the incidence of future cardiovascular and cerebrovascular events.[12]Ogden LG, He J, Lydick E, et al. Long-term absolute benefit of lowering blood pressure in hypertensive patients according to the JNC VI risk stratification. Hypertension. 2000 Feb;35(2):539-43.
http://hyper.ahajournals.org/cgi/content/full/35/2/539
http://www.ncbi.nlm.nih.gov/pubmed/10679494?tool=bestpractice.com
[13]D'Anci KE, Tipton K, Hedden-Gross A, et al. Effect of intensive blood pressure lowering on cardiovascular outcomes: a systematic review prepared for the 2020 U.S. Department of Veterans Affairs/U.S. Department of Defense Guidelines. Ann Intern Med. 2020 Dec 1;173(11):895-903.
http://www.ncbi.nlm.nih.gov/pubmed/32866419?tool=bestpractice.com
The aim of early diagnosis and treatment of hypertension is to lower overall cardiovascular risk and prevent cerebrovascular events.
The effects of chronic hypertension on organ systems are referred to as hypertension-mediated organ damage.
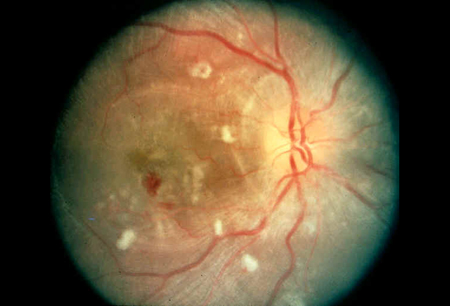
Left ventricular hypertrophy, cardiovascular disease, cerebrovascular disease, hypertensive retinopathy, and nephropathy are the most common manifestations.[14]Nadar SK, Tayebjee MH, Meserelli F, et al. Target organ damage in hypertension: pathophysiology and implications for drug therapy. Curr Pharm Des. 2006;12(13):1581-92.
http://www.ncbi.nlm.nih.gov/pubmed/16729871?tool=bestpractice.com
The presence of left ventricular hypertrophy is a poor prognostic sign, and regression of left ventricular hypertrophy improves prognosis.[15]Lewington S, Clarke R, Qizilbash N, et al. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002 Dec 14;360(9349):1903-13.
http://www.ncbi.nlm.nih.gov/pubmed/12493255?tool=bestpractice.com
Patients with resistant hypertension are at higher risk of experiencing cardiovascular and cerebrovascular events and developing chronic kidney disease.[16]Carey RM, Calhoun DA, Bakris GL, et al. Resistant hypertension: detection, evaluation, and management: a scientific statement from the American Heart Association. Hypertension. 2018 Nov;72(5):e53-90.
https://www.ahajournals.org/doi/full/10.1161/HYP.0000000000000084
http://www.ncbi.nlm.nih.gov/pubmed/30354828?tool=bestpractice.com
Cardiovascular risk
Guidelines on the management of hypertension emphasize the importance of calculating and managing the overall cardiovascular risk of a patient, rather than focusing only on blood pressure readings. The ACC and AHA have published an online tool to calculate patients’ 10-year and lifetime risk of atherosclerotic cardiovascular disease.
ACC: ASCVD Risk Estimator Plus
Opens in new window
For individuals ages 40-70 years, each increment of 20 mmHg in systolic blood pressure or 10 mmHg in diastolic blood pressure across the entire blood pressure range from 115/75 to 185/115 mmHg doubles the risk of cardiovascular disease.[17]Blair SN, Goodyear NN, Gibbons LW, et al. Physical fitness and incidence of hypertension in healthy normotensive men and women. JAMA. 1984 Jul 27;252(4):487-90.
http://www.ncbi.nlm.nih.gov/pubmed/6737638?tool=bestpractice.com
The European Society for Cardiology has proposed that sex-specific thresholds may be appropriate as lower blood pressure levels are associated with an increased risk of cardiovascular disease in women.[18]Gerdts E, Sudano I, Brouwers S, et al. Sex differences in arterial hypertension. Eur Heart J. 2022 Dec 7;43(46):4777-88.
https://academic.oup.com/eurheartj/article/43/46/4777/6711154?login=false
http://www.ncbi.nlm.nih.gov/pubmed/36136303?tool=bestpractice.com
Treating associated cardiovascular risk factors such as obesity, diabetes, hypercholesterolemia, and smoking are as important as managing hypertension in lowering overall cardiovascular risk.
Войдите в учетную запись или оформите подписку, чтобы получить полноценный доступ к BMJ Best Practice