Summary
Definition
History and exam
Key diagnostic factors
- abdominal pain
- abdominal tenderness
- presence of risk factors
Other diagnostic factors
- haematochezia/melaena
- diarrhoea
- nausea
- weight loss
- abdominal bruit
- vasculitis
- light headedness, pallor, dyspnoea
- food fear (sitophobia)
Risk factors
- old age
- history of smoking
- hypercoagulable states
- atrial fibrillation
- myocardial infarction
- structural heart defects
- history of vasculitis
- recent cardiovascular surgery
- shock
- congestive heart failure
- atherosclerosis
- irritable bowel syndrome
- colonic carcinoma
- constipation
- long-term laxative use
- use of vasopressors, digoxin, cocaine
Diagnostic investigations
1st investigations to order
- CT scan with contrast/CT angiogram
- FBC
- arterial blood gases and serum lactate
- urea and electrolytes
- liver function tests
- CRP
- coagulation studies, group and save and crossmatch
- ECG
- erect CXR
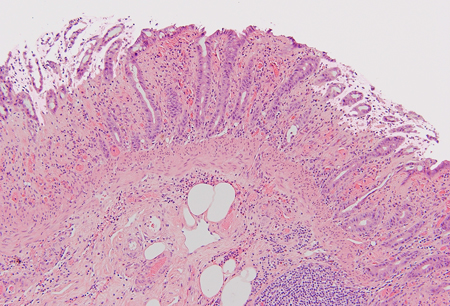
- sigmoidoscopy or colonoscopy
- upper gastrointestinal endoscopy
- D-dimer
Investigations to consider
- mesenteric angiography
- mesenteric duplex ultrasound
- magnetic resonance angiography
- amylase
- studies for ova, cysts, and parasites
- faecal culture
- Clostridium difficile toxin assay
- abdominal x-rays
Treatment algorithm
evidence of infarction, perforation, or peritonitis on diagnostic computed tomography scan
no evidence of infarction, perforation, or peritonitis on diagnostic computed tomography scan
chronic mesenteric ischaemia
ischaemic colitis
non-acute colonic ischaemia
Contributors
Expert advisers
Jennifer Straatman
Consultant Upper GI surgeon
Queen Alexandra Hospital
Portsmouth
UK
Disclosures
JS declares that she has no competing interests.
Acknowledgements
BMJ Best Practice would like to gratefully acknowledge the previous expert contributors, whose work has been retained in parts of the content:
Alex von Roon, MB, ChB, PhD, FRCS
Clinical Senior Lecturer
Honorary Consultant Colorectal Surgeon
Department of Surgery and Cancer
Imperial College London
London
UK
James Lewis, MBBS, BSc, MRCS
Clinical Research Fellow
Department of Surgery and Cancer
Imperial College London
London
UK
John Abercrombie FRCS
General and Colorectal Surgeon
Queen’s Medical Centre
Nottingham
UK
Disclosures
AVR and JL declare that they have no competing interests. JA is a member of the Council of The Royal College of Surgeons of England and Clinical Lead for General Surgery, Getting It Right First Time. JA provides expert advice regarding suitability of surgical treatments for Spire Healthcare.
Peer reviewers
Frances Howse, MA (Oxon), BM (Hons), FRCS (Eng)
Consultant
Acute and General Surgery
University Hospital Southampton NHS Foundation Trust
Southampton
UK
Disclosures
FH declares that she has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Bala M, Catena F, Kashuk J, et al. Acute mesenteric ischemia: updated guidelines of the World Society of Emergency Surgery. World J Emerg Surg. 2022 Oct 19;17(1):54.Full text Abstract
Tilsed JV, Casamassima A, Kurihara H, et al. ESTES guidelines: acute mesenteric ischaemia. Eur J Trauma Emerg Surg. 2016 Apr;42(2):253-70.Full text Abstract
Terlouw LG, Moelker A, Abrahamsen J, et al. European guidelines on chronic mesenteric ischaemia: joint United European Gastroenterology, European Association for Gastroenterology, Endoscopy and Nutrition, European Society of Gastrointestinal and Abdominal Radiology, Netherlands Association of Hepatogastroenterologists, Hellenic Society of Gastroenterology, Cardiovascular and Interventional Radiological Society of Europe, and Dutch Mesenteric Ischemia Study group clinical guidelines on the diagnosis and treatment of patients with chronic mesenteric ischaemia. United European Gastroenterol J. 2020 May;8(4):371-95.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Infectious colitis
- Ulcerative colitis
- Crohn's disease
More DifferentialsGuidelines
- Acute mesenteric ischemia
- ESTES guidelines: acute mesenteric ischaemia
More GuidelinesVideos
How to perform an ECG animated demonstration
Venepuncture and phlebotomy animated demonstration
More videosPatient information
Ischaemic bowel disease: what is it?
Ischaemic bowel disease: what are the treatment options?
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer
