Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- dyspnea
- productive cough
- fever
Outros fatores diagnósticos
- chest pain
- asymmetric expansion of the chest
- diminished resonance
- egophony
- whisper pectoriloquy
- crackles or rhonchi
- tachycardia
- malaise/anorexia
Fatores de risco
- poor infection control/hand hygiene
- intubation and mechanical ventilation; endotracheal cuff pressure <20 cm H₂O
- supine position
- poor oral hygiene
- sedation/no interruption in sedation
- intubation/reintubation
Investigações diagnósticas
Primeiras investigações a serem solicitadas
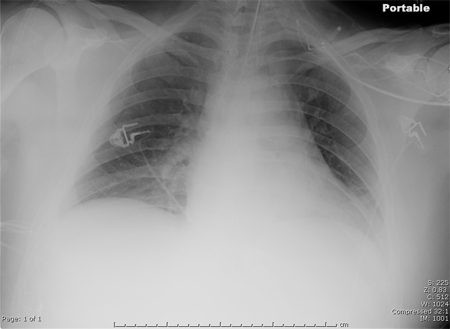
- chest x-ray
- WBC count with differential
- pulse oximetry
- culture of lower respiratory tract sample
Investigações a serem consideradas
- ABG
- diagnostic thoracentesis
- CT chest
- CRP
- lung ultrasound
Novos exames
- MRSA nasal swab
Algoritmo de tratamento
before culture results: without risk factors for multidrug-resistant (MDR) pathogen
before culture results: with risk factors for multidrug-resistant (MDR) pathogen, including Pseudomonas and MRSA
after culture results: due to gram-negative pathogen
after culture results: due to gram-positive pathogen
Colaboradores
Consultores especialistas
Forest W. Arnold, DO, MSc, FIDSA
Professor of Medicine
Chief, Division of Infectious Diseases
Director Infectious Diseases Fellowship Training Program
Department of Medicine
School of Medicine
University of Louisville
Louisville
KY
Declarações
FWA declares that he has no competing interests.
Revisores
Krishna Sundar, MD, FCCP
Associate Professor (Clinical)
Department of Medicine
University of Utah
Director
Pulmonary and Critical Care Research
IHC Urban South
Utah Valley Pulmonary Clinic
UT
Declarações
KS declares that he has no competing interests.
Ozan Akca, MD
Director of Research
Associate Professor
Department of Anesthesiology and Perioperative Medicine
Neuroscience and Anesthesia Intensive Care Unit
University of Louisville
Louisville
KY
Declarações
OA declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016 Sep 1;63(5):e61-111.Texto completo Resumo
Klompas M, Branson R, Cawcutt K, et al. Strategies to prevent ventilator-associated pneumonia, ventilator-associated events, and nonventilator hospital-acquired pneumonia in acute-care hospitals: 2022 Update. Infect Control Hosp Epidemiol. 2022 Jun;43(6):687-713.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Coronavirus disease 2019 (COVID-19)
- Cardiogenic pulmonary edema
- Acute respiratory distress syndrome
Mais Diagnósticos diferenciaisDiretrizes
- Strategies to prevent ventilator-associated pneumonia, ventilator-associated events, and nonventilator hospital-acquired pneumonia in acute-care hospitals
- Management of adults with hospital-acquired and ventilator-associated pneumonia
Mais DiretrizesVideos
Supraglottic airway devices: animated demonstration
Nasopharyngeal airway: animated demonstration
Mais vídeosFolhetos informativos para os pacientes
Pneumonia
Mais Folhetos informativos para os pacientesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal