Resumo
Definição
História e exame físico
Principais fatores diagnósticos
- cough
- dyspnea
Outros fatores diagnósticos
- fever
- pleuritic chest pain
- tachypnea
- foul-smelling breath
- crepitations
- frothy or purulent sputum
- history of vomiting
Fatores de risco
- chemoradiation for head and neck cancers
- altered mental status
- swallowing dysfunction
- gastrointestinal disease
- intubation or tracheostomy tube
- older age
- poor oral hygiene
- feeding tube
- recumbent position
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- O2 saturation
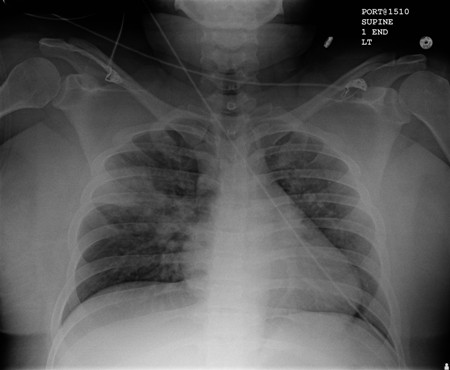
- CXR
- CBC
- sputum Gram stain
- sputum culture
Investigações a serem consideradas
- point-of-care lung ultrasound
- ABG
- bronchoscopy
Algoritmo de tratamento
all patients
Colaboradores
Consultores especialistas
Michael J. Lanspa, MD, MS
Adjunct Associate Professor
Division of Pulmonary and Critical Care Medicine
Intermountain Medical Center
University of Utah
Salt Lake City
UT
Declarações
MJL declares that he has no competing interests.
Agradecimentos
Dr Michael J. Lanspa would like to gratefully acknowledge Dr Richard Kanner and Dr Krishna Sundar, previous contributors to this topic.
Declarações
DK and KS declare that they have no competing interests.
Revisores
Toby Maher, MB, PhD, MRCP
Consultant Respiratory Physician
Department of Respiratory Medicine
Royal Brompton Hospital
London
UK
Declarações
TM has received research funding from the Wellcome Trust and GlaxoSmithKline. He has acted as a paid consultant to GSK, Actelion, and Respironies.
Feras Hawari, MD
Chief of Pulmonary and Critical Care
King Hussein Cancer Center
Amman
Jordan
Declarações
FH declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019 Oct 1;200(7):e45-e67.Texto completo Resumo
American Society of Anesthesiologists. Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures: an updated report by the American Society of Anesthesiologists Task Force on Preoperative Fasting and the Use of Pharmacologic Agents to Reduce the Risk of Pulmonary Aspiration. Anesthesiology. 2017 Mar;126(3):376-93.Texto completo Resumo
Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016 Sep 1;63(5):e61-e111.Texto completo Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Differentials
- Aspiration pneumonitis
- Atelectasis
- Pulmonary edema
Mais DifferentialsGuidelines
- Diagnosis and treatment of adults with community-acquired pneumonia
- Practice guidelines for preoperative fasting and the use of pharmacologic agents to reduce the risk of pulmonary aspiration: application to healthy patients undergoing elective procedures
Mais GuidelinesPatient information
Pneumonia
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer