Summary
Definition
History and exam
Key diagnostic factors
- exertional dyspnea
Other diagnostic factors
- orthopnea
- paroxysmal nocturnal dyspnea
- abdominal fullness
- rales
- jugular venous distention
- hepatojugular reflux
- congestive hepatomegaly
- lower extremity edema
- laterally displaced apical impulse
- gallop sounds
Risk factors
- hypertension
- atrial fibrillation (AF)
- female sex
- age >70 years
- obesity
- coronary artery disease (CAD)/ischemia
- diabetes mellitus
- chronic kidney disease (CKD)
- dyslipidemia
- exposure to cardiotoxic agents
- metabolic syndrome or cardiovascular-kidney-metabolic (CKM) syndrome
- myocardial and pericardial disorders
- obstructive sleep apnea
Diagnostic investigations
Исследования, которые показаны в первую очередь
- serum electrolytes
- renal function tests
- liver enzymes
- B-natriuretic peptide (BNP)/N-terminal prohormone B-natriuretic peptide (NT-proBNP)
- CBC and iron studies
- 12-lead ECG
- blood glucose
- thyroid function tests
- blood lipids
- CXR
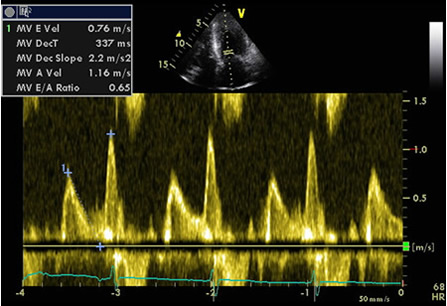
- transthoracic echocardiography
Исследования, проведение которых нужно рассмотреть
- cardiac magnetic resonance (CMR) imaging
- CT angiography
- radionuclide ventriculography (MUGA scan)
- stress testing
- cardiopulmonary exercise testing (CPET)
- cardiac catheterization and coronary angiography
Алгоритм лечения
all patients
Составители
Авторы
Syed Wamique Yusuf, FACC, FRCPI
Professor of Medicine
Department of Cardiology
University of Texas MD Anderson Cancer Center
Houston
TX
Раскрытие информации
SWY declares that he has no competing interests.
Carl Zehner, MD
Assistant Professor of Medicine
Department of Cardiology
University of Texas MD Anderson Cancer Center
Houston
TX
Disclosures
CZ declares that he has no competing interests.
Acknowledgements
Dr Syed Wamique Yusuf and Dr Carl Zehner would like to gratefully acknowledge Dr Gerald Carr-White, Dr Jessica Webb, Dr Gerard Aurigemma, Dr Lokesh Tejwani, Dr Marc E. Del Rosario, and Dr Kul Aggarwal, previous contributors to this topic.
Disclosures
GCW has been reimbursed by Pfizer, AstraZeneca, Bayer, Medtronic, St Jude, and Sanofi for attending conferences. He has attended Advisory Boards for Medtronic, St Jude, Novartis, Shire, Sanofi, and Servier. JW has a joint working venture with BI for a community pharmacist post. GA, LT, MEDR, and KA declare that they have no competing interests.
Peer reviewers
Edward Geltman, MD
Professor of Medicine
Cardiovascular Division
Washington University School of Medicine
St. Louis
MO
Disclosures
EG has lectured for Novartis, Forest, Merck, and Pfizer.
Jerry Murphy, MB, BS, DM, FRCP
Consultant Cardiologist
Darlington Memorial Hospital
Darlington
UK
Disclosures
Not disclosed.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Bozkurt B, Coats AJ, Tsutsui H, et al. Universal definition and classification of heart failure: a report of the Heart Failure Society of America, Heart Failure Association of the European Society of Cardiology, Japanese Heart Failure Society and Writing Committee of the Universal Definition of Heart Failure. 2021 Mar 1;S1071-9164(21)00050-6.Full text Abstract
Kittleson MM, Panjrath GS, Amancherla K, et al. 2023 ACC expert consensus decision pathway on management of heart failure with preserved ejection fraction: a report of the American College of Cardiology Solution Set Oversight Committee. J Am Coll Cardiol. 2023 May 9;81(18):1835-78.Full text Abstract
Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA guideline for the management of heart failure: a report of the American College of Cardiology/American Heart Association Joint Committee on clinical practice guidelines. Circulation. 2022 May 3;145(18):e895-1032.Full text Abstract
McDonagh TA, Metra M, Adamo M, et al. 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2021 Sep 21;42(36):3599-726.Full text
McDonagh TA, Metra M, Adamo M, et al. 2023 focused update of the 2021 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2023 Oct 1;44(37):3627-39.Full text
Borlaug BA, Sharma K, Shah SJ, et al. Heart failure with preserved ejection fraction: JACC scientific statement. J Am Coll Cardiol. 2023 May 9;81(18):1810-34. Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Heart failure with reduced ejection fraction
- Cardiac amyloidosis
- Hypertrophic cardiomyopathy (HCM)
More DifferentialsGuidelines
- 2024 ACC expert consensus decision pathway on clinical assessment, management, and trajectory of patients hospitalized with heart failure focused update: a report of the American College of Cardiology Solution Set Oversight Committee
- ACR appropriateness criteria: suspected and known heart failure
More GuidelinesPatient information
Heart failure
Heart failure: how can I help myself?
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer