Summary
Definition
History and exam
Key diagnostic factors
- male sex
- age <30 years
- meningismus
- headache
- cranial nerve palsy
- positive Kernig or Brudzinski sign
- fever
- increased head circumference (infants)
- bulging fontanelles (infants)
Other diagnostic factors
- neurological deficit
- papilledema
Risk factors
- sinusitis
- otitis media
- dental procedure/infection
- meningitis
- recent head and neck surgery or neurosurgery
- congenital heart disease
- endocarditis
- diverticular disease
- hereditary hemorrhagic telangiectasia or arteriovenous malformation
- diabetes mellitus
- HIV or immunocompromise
- intravenous drug use
- chronic granulomatous disease
- hemodialysis
- birth prematurity
- cystic fibrosis
Diagnostic tests
1st tests to order
- CBC
- serum erythrocyte sedimentation rate (ESR)
- serum CRP
- serum PT, PTT, and INR
- blood culture
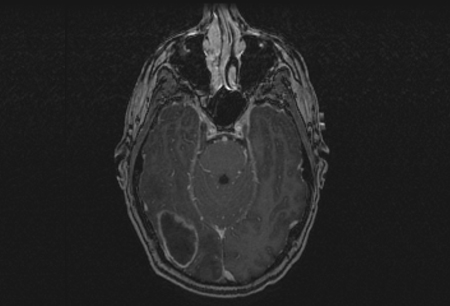
- MRI with contrast
- CT head with and without contrast
- ultrasound head (infants)
Tests to consider
- serum toxoplasma titer
- magnetic resonance spectroscopy (MRS)
- lumbar puncture (LP) with cerebrospinal fluid (CSF) analysis
- CT chest, abdomen, and pelvis
- bone scan
- mammogram
Treatment algorithm
presumed brain abscess
suspected or confirmed bacterial etiology
confirmed fungal etiology
suspected or confirmed parasitic etiology
cryptogenic brain abscess
Contributors
Authors
Walter A. Hall, MD, MBA
Professor
Department of Neurosurgery
SUNY Upstate Medical University
Syracuse
NY
Disclosures
WAH is an author of a number of references cited in this topic.
Acknowledgements
Dr Walter A. Hall would like to gratefully acknowledge Dr Peter D. Kim, a previous contributor to this topic. PDK declares that he has no competing interests.
Peer reviewers
Stephen Haines, MD
Professor and Head
Department of Neurosurgery
University of Minnesota
Minneapolis
MN
Disclosures
SH and WAH were colleagues on a faculty of the University of Minnesota between 1991 and 1997 and again between 2004 and 2006. They have coauthored articles on neurosurgical infection.
Sabrina Ravaglia, MD, PhD
Staff Physician
Department of Neurological Sciences
Institute of Neurology C. Mondino
Pavia
Italy
Disclosures
SR declares that she has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Hall WA, Truwit CL. The surgical management of infections involving the cerebrum. Neurosurgery. 2008 Feb;62(2 suppl):519-30. Abstract
Brouwer MC, Coutinho JM, van de Beek D. Clinical characteristics and outcome of brain abscess: systematic review and meta-analysis. Neurology. 2014 Mar 4;82(9):806-13. Abstract
Goodkin HP, Harper MB, Pomeroy SL. Intracerebral abscess in children: historical trends at Children's Hospital Boston. Pediatrics. 2004 Jun;113(6):1765-70. Abstract
Expert Panel on Neurologic Imaging; Whitehead MT, Cardenas AM, et al. ACR Appropriateness Criteria® headache. J Am Coll Radiol. 2019 Nov;16(11s):S364-77.Full text Abstract
American College of Radiology. ACR-ASNR-SPR practice parameter for the performance and interpretation of magnetic resonance spectroscopy of the central nervous system. 2019 [internet publication].Full text
Infection in Neurosurgery Working Party of the British Society for Antimicrobial Chemotherapy. The rational use of antibiotics in the treatment of brain abscess. Br J Neurosurg. 2000 Dec;14(6):525-30. Abstract
Mampalam TJ, Rosenblum ML. Trends in the management of bacterial brain abscesses: a review of 102 cases over 17 years. Neurosurgery. 1988 Oct;23(4):451-8. Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Primary central nervous system neoplasm
- Metastatic lesion
- Recurrent tumor/radiation necrosis in a postsurgical patient
More DifferentialsLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer