Diferenciales
Común
Constipation
Antecedentes
poor diet and fluid intake; history of cerebral palsy, learning difficulties, or spinal cord problems; psychological factors (e.g., depression, abuse, ADHD, autism, oppositional disorder), weaning, toilet training, start of schooling or other causes of stress may be present; vague abdominal pain, painful defecation (infants may extend their legs and squeeze anal and buttock muscles to prevent stooling; toddlers often rise up on their toes, shift back and forth, and stiffen their legs and buttocks), faecal incontinence; medication with known constipating agents (e.g., iron supplements); obesity, low birth weight
Examen
examination findings may be minimal (mild abdominal tenderness, stool in rectum); abdominal distension in severe cases or in small children; faecal mass palpable on abdominal examination; absence of peritonitis (guarding or rebound tenderness); sacral dimples or pits and/or tags/tufts indicative of spinal cord abnormality (i.e., spina bifida); anal fissure, haemorrhoids (rare in children; may be mistaken for skin tags from Crohn's disease); imperforate anus or anal stenosis
Primera prueba diagnóstica
- none:
clinical diagnosis
Más
Otras pruebas diagnósticas
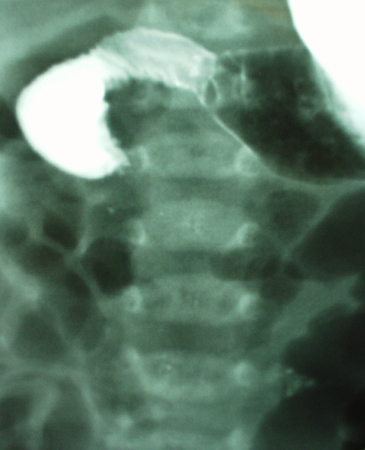
- abdominal x-ray:
stool visible throughout colon
Más - radiopaque marker colonic transit study:
slow colonic transit, as measured by delay in marker movement, confirms constipation
Acute appendicitis
Antecedentes
history of sharp or stabbing periumbilical pain that migrates to the right lower quadrant (RLQ); anorexia, fever, vomiting, and/or diarrhoea may be present; occurs in all age groups but is rare in infants
Examen
patient lies still, tries not to move (especially in severe cases with significant peritoneal irritation); positive McBurney's sign (RLQ pain and tenderness to palpation at a point two-thirds along a line from the umbilicus to the anterior superior iliac spine); positive Rovsing's sign (pain in the RLQ in response to left-sided palpation, suggesting peritoneal irritation); positive psoas sign (pain in the RLQ when child placed on left side and right hip gently hyperextended, suggesting irritation to the psoas fascia and muscle); positive obturator sign (RLQ pain on internal rotation of the flexed right thigh); rectal tenderness and/or palpable abscess in RLQ
Primera prueba diagnóstica
Other investigations
- abdominal ultrasound:
dilated appendix, free fluid; appendicolith may be present
More - CT scan abdomen and pelvis:
dilated appendix, free fluid, mesenteric stranding, or appendicolith; abscess or phlegmon consistent with perforated appendicitis
More - MRI scan abdomen and pelvis:
dilated appendix; hyperintensity of the luminal contents of the appendix, periappendiceal tissue and thickened wall
More
Gastroenteritis
ანამნეზი
vague abdominal pain with nausea and vomiting; diarrhoea with or without mucus in stool; recent travel or contact with sick individual(s) or ingestion of suspected food and drink; >10 days suggests parasitic or non-infectious cause; fever, chills, myalgia, rhinorrhoea, upper respiratory symptoms
გასინჯვა
diffuse abdominal pain without evidence of peritonitis (no guarding or rebound tenderness); abdominal distension; hyperactive bowel sounds; mucus in stool (bacterial or parasitic); signs of volume depletion (tachycardia, hypotension, dry mucous membranes, poor capillary refill, sunken fontanelle in infants); low-grade fever, lethargy and/or irritability, reduced response to noxious stimuli, abnormal temperature (raised or low)
პირველი გამოკვლევა
- none:
clinical diagnosis
სხვა გამოკვლევები
- serum electrolytes:
normal or low sodium and potassium
მეტი - urea and creatinine:
normal; may have evidence of renal failure in patients with haemolytic uraemic syndrome
მეტი - stool microscopy and culture:
faecal leukocytes; ova or parasites; culture positive for infectious agent in bacterial gastroenteritis
მეტი - urine dipstick:
may detect presence of albumin or blood in haemolytic uraemic syndrome
- FBC:
variable
მეტი - blood culture:
may be positive for infectious agent in presence of sepsis
მეტი - endoscopy with biopsy:
variable
მეტი
Urinary tract infection
ანამნეზი
neonates and infants: fever, vomiting, lethargy, irritability, and poor feeding; older children: dysuria, urinary frequency and urgency, back pain if pyelonephritis
გასინჯვა
variable; fever >39°C (>102.2°F); suprapubic and/or costovertebral angle tenderness; irritability; foul-smelling urine; gross haematuria
პირველი გამოკვლევა
其他检查
- renal ultrasound:
abnormalities may be present such as dilatation of the renal pelvis or ureters, or distension of thick-walled bladder; renal abscess: area of radiolucency to the renal parenchyma with local hypoperfusion on colour Doppler; perinephric abscess: hypoechoic fluid
更多 - voiding cystourethrogram (VCUG):
if vesicoureteral reflux is present: contrast seen ascending out of the bladder into the upper urinary tract
更多
Abdominal trauma (blunt or penetrating)
病史
history of trauma; may have multiple complaints; history may suggest child abuse or non-accidental trauma (e.g., inconsistent or changing history, history not consistent with injuries/examination)
检查
abdominal tenderness; skin marks reflecting mechanism of injury (e.g., seat belt mark); referred left shoulder pain (due to splenic injury); blood at the urethral meatus, or haematuria (indicate urinary tract or kidney injury); signs of non-accidental trauma may be present (e.g., cigarette burns, subdural haemorrhages in an infant/young toddler)
首要检查
Cholelithiasis/cholecystitis
História
recurrent, episodic right upper quadrant (RUQ) pain, may radiate to the back and is classically colicky in nature; often occurs after eating, particularly fatty foods; nausea, vomiting, and anorexia may be present; persistent pain and fever may signify acute cholecystitis; referred pain to right shoulder can occur; presence of risk factors (e.g., sickle cell disease, cystic fibrosis)
Exame físico
right subcostal region tenderness; positive Murphy's sign (during palpation, deep inspiration causes pain to suddenly become worse and produces inspiratory arrest); palpable distended, tender gallbladder; fever suggests acute cholecystitis; jaundice rare and suggests common bile duct obstruction
Primeira investigação
- RUQ ultrasound:
gallstones; ductal dilation, thickened gallbladder wall (>4 mm); pericholecystic fluid; may also see ultrasonographic Murphy's sign
- liver tests:
may see raised alk phos, bilirubin, and aminotransferase
Mais - FBC:
normal WBC (suggests cholelithiasis) or leukocytosis (suggests acute cholecystitis)
- C-reactive protein:
normal (suggests cholelithiasis) or raised (suggests acute cholecystitis)
Primary dysmenorrhoea
História
history of recurrent crampy abdominal pain associated with menstruation
Exame físico
lower abdominal tenderness; normal pelvic examination
Primeira investigação
- none:
diagnosis is clinical
Outras investigações
- abdominal/pelvic ultrasound:
normal; however, useful to rule out other diagnoses
Pneumonia
História
cough; purulent sputum production; upper respiratory tract symptoms (rhinorrhoea, sore throat, nasal congestion), shortness of breath, fever, and chills; splinting secondary to pain; vomiting, diarrhoea, anorexia
Exame físico
tachypnoea, cyanosis, decreased breath sounds, crackles/rales on auscultation, dullness on percussion; abdominal tenderness and distension without guarding or rebound
Primeira investigação
- FBC:
variable
更多 - chest x-ray:
infiltration, consolidation, effusion
- sputum culture:
growth of infecting organism
Functional abdominal pain
病史
history may be acute, chronic, or cyclic (frequently girls aged 8-12 years), complaint of vague, persistent, central abdominal pain common, may be associated nausea and vomiting, particularly in chronic cases; family history of functional disorders common (e.g., irritable bowel syndrome, anxiety, psychiatric disorders, and migraine); Rome IV criteria use symptoms for diagnosis
检查
periumbilical tenderness, abdomen is soft, non-distended, no guarding or rebound tenderness; examination of other systems normal
首要检查
- none:
diagnosis is clinical after exclusion of possible organic causes
其他检查
- FBC:
normal
- erythrocyte sedimentation rate:
normal
- urinalysis:
normal
- stool microscopy:
normal
Infantile colic
病史
paroxysms of uncontrollable crying in otherwise healthy and well-fed infant aged <5 months; duration of crying is >3 hours per day, and >3 days per week, for at least 3 weeks; sibling(s) may have history of infantile colic
检查
examination findings may be minimal; infant typically well and thriving
首要检查
- none:
clinical diagnosis
更多
不常见
Intussusception
病史
usually infant between 3 months and 12 months of age presenting with colicky abdominal pain, flexing of the legs, fever, lethargy, and vomiting; Henoch-Schonlein purpura (HSP) may be initiating factor in an older child (usually <11 years of age); vague abdominal complaints; severe, cramp-like abdominal pain; child may be inconsolable
检查
may see gross or occult blood that may be mixed with mucus and have red-brick-coloured jelly-like appearance, abdominal tenderness, and palpable abdominal mass; signs of HSP may be present in older child (rash of palpable purpura, blood in the stools)
首要检查
Other investigations
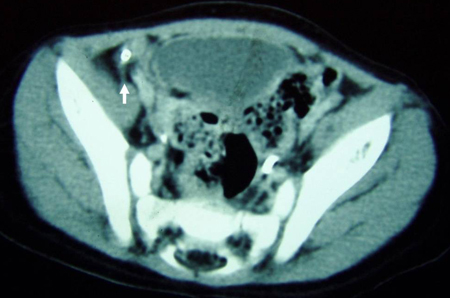
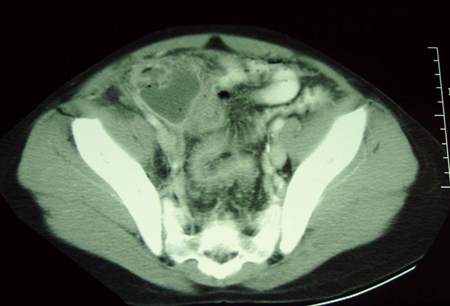
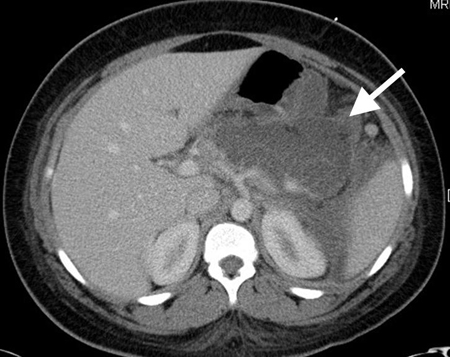
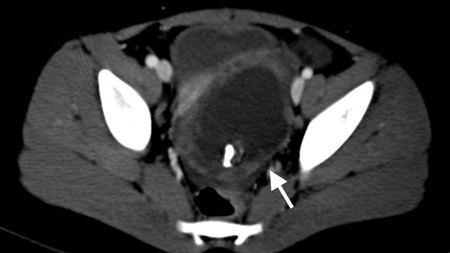
- CT scan abdomen and pelvis:
target lesion: intraluminal soft-tissue density mass with an eccentrically placed fatty area; reniform mass: high attenuation peripherally and lower attenuation centrally; sausage-shaped mass: alternating areas of low and high attenuation representing closely spaced bowel wall, mesenteric fat and/or intestinal fluid and gas
More - FBC:
may show raised WBC (suggests intestinal ischaemia)
- faecal occult blood test:
positive test can support suspicion of intussusception
More
Meckel's diverticulum
History
typically aged <2 years; may present with abdominal pain (may be intermittent or mimic acute appendicitis), and/or painless passage of bright red blood per rectum (haematochezia); often asymptomatic
Exam
painless dark red, maroon, or red-brick-coloured jelly-like stools; abdominal tenderness with guarding and rebound (may suggest diverticulitis); palpable abdominal mass (may suggest intussusception)
1st investigation
Other investigations
- CT scan abdomen and pelvis:
may show intussusception, Meckel's diverticulitis, and/or dilated bowel consistent with bowel obstruction
More
Mesenteric adenitis
History
diffuse abdominal pain; history of recent or current upper respiratory tract infection
检查
fever, abdominal tenderness not localised to right lower quadrant, rhinorrhoea, hyperaemic pharynx or oropharynx (pharyngitis), and/or associated extramesenteric lymphadenopathy (usually cervical)
首要检查
- abdominal ultrasound:
enlarged mesenteric lymph nodes
更多
其他检查
- CT scan abdomen and pelvis:
enlarged mesenteric lymph nodes
更多
Hirschsprung's disease
病史
males affected more commonly, mainly presents in early infancy (prior to 6 months); failure to pass meconium in first 36 hours of life strongly suggestive; increased incidence in Down syndrome
检查
abdominal distension, fullness in left lower quadrant; palpable faecal mass on abdomen examination; absence of peritonitis (no guarding or rebound tenderness); small rectum and absence of stool on rectal examination (should be performed by clinician able to interpret features of Hirschsprung's disease); dysmorphic features of Down syndrome may be present
首要检查
Ulcerative colitis
病史
positive family history, bloody diarrhoea, cramping abdominal pain, anorexia, weight loss, fever, rash
检查
evidence of weight loss, pallor, abdominal tenderness, abdominal mass, iritis (inflamed irritated eyes), arthritis, sacroiliitis, erythema nodosum, pyoderma gangrenosum
首要检查
- faecal calprotectin:
raised
更多 - FBC:
leukocytosis, anaemia, thrombocytosis
更多 - colonoscopy with biopsy:
continuous uniform rectal involvement, loss of vascular marking, diffuse erythema, mucosal granularity and friability, mucosal oedema ulcers, fistulas (rarely seen), normal terminal ileum (or mild backwash ileitis in pancolitis)
更多 - erythrocyte sedimentation rate:
raised
更多 - C-reactive protein:
raised
更多
其他检查
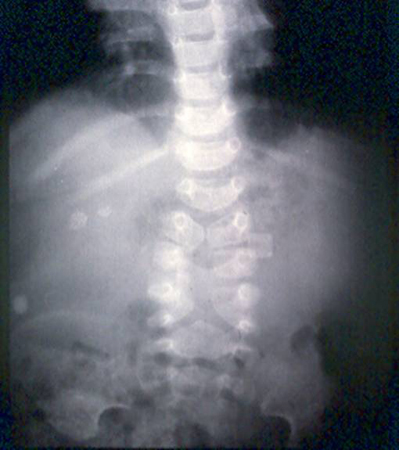
- plain abdominal x-rays:
dilated loops with air-fluid level secondary to ileus; free air is consistent with perforation; in toxic megacolon, the transverse colon is dilated to 6 cm or more in diameter
更多 - CT scan abdomen:
thickened inflamed bowel mucosa, thumbprinting, intestinal dilation or evidence of stricture; inflamed mesentery; intra-abdominal abscesses
更多 - serologic markers: perinuclear antineutrophil cytoplasmic antibody (pANCA) and anti-Saccharomyces cerevisiae antibody (ASCA):
positive pANCA
更多
Crohn's disease
病史
crampy abdominal pain, intermittent diarrhoea, bloody diarrhoea if colitis a feature (blood less common in Crohn's disease than in ulcerative colitis), weight loss, fatigue, family history of inflammatory bowel disease
检查
aphthous ulcers, evidence of weight loss, pallor, abdominal tenderness, abdominal mass, perianal fistula, perirectal abscess, anal fissure, perianal skin tags; extraintestinal manifestations including iritis, arthritis, sacroiliitis, erythema nodosum, pyoderma gangrenosum
首要检查
- faecal calprotectin:
may be raised
更多 - FBC:
leukocytosis, anaemia, thrombocytosis
更多 - C-reactive protein:
raised
更多 - erythrocyte sedimentation rate:
raised
更多 - colonoscopy with biopsy:
may demonstrate inflammation, friability, ulcer formation, and oedema
更多 - MR enterography:
skip lesions, bowel wall thickening, surrounding inflammation, abscess, fistulas
其他检查
- plain abdominal x-rays:
small bowel or colonic dilation; calcification; intra-abdominal abscesses
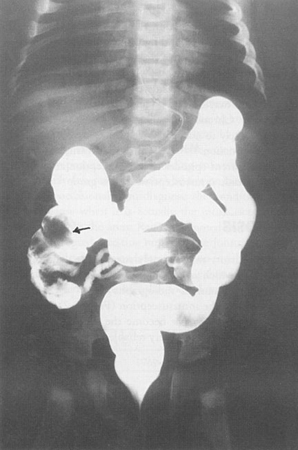
更多 - upper gastrointestinal series with small bowel follow-through:
oedema and ulceration of the mucosa with luminal narrowing and strictures
更多 - CT scan abdomen and pelvis:
skip lesions, bowel wall thickening, surrounding inflammation, abscess, fistulas
更多 - serological markers: perinuclear antineutrophil cytoplasmic antibody (pANCA) and anti-Saccharomyces cerevisiae antibody (ASCA):
positive ASCA
更多
Small bowel obstruction
病史
intolerant of feeding, with nausea and/or bilious vomiting; abdominal pain may or may not be a feature; history of previous abdominal surgery; history of cystic fibrosis may be present
检查
limited abdominal distension (with proximal obstructions in the duodenum or early jejunum); abdominal tenderness may or may not be present; rebound tenderness and guarding may occur if perforation, ischaemia, and peritonitis; hyperactive bowel sounds (early finding), hypoactive or absent bowel sounds (late finding); incarcerated femoral, obturator, umbilical or ventral hernia may be present
首要检查
- abdominal x-ray:
dilated small bowel loops, air-fluid levels throughout abdomen
更多
其他检查
- abdominal ultrasound:
may demonstrate focal area causing obstruction
更多 - upper gastrointestinal contrast study:
dilated small intestine; may demonstrate a transition zone of obstruction
More - lower gastrointestinal contrast study:
dilated small intestine; may demonstrate a transition zone of obstruction
More - CT scan abdomen:
dilated small intestine; may demonstrate a transition zone of obstruction, mass, tumour, abscess
More
Volvulus
History
infant age group; history of bilious vomiting; pain usually manifests as notable transition to an inconsolable state
Exam
often diffuse abdominal distension and tenderness; faint or no bowel sounds, rigid abdomen, guarding, rebound tenderness, fever, or haematochezia
1st investigation
Other investigations
- CT scan abdomen:
bowel obstruction with whirl pattern of mesentery
More
Large bowel obstruction
History
history of risk factors: neurodevelopmental problems, inflammatory bowel disease, diabetes, poor diet, previous colorectal resection, laxative misuse, megacolon, or previous abdominal surgery; change in bowel habit with partial or complete obstruction, or change in calibre of stool; colicky abdominal pain becoming more constant and worse with movement, coughing or deep breathing as bowel approaches perforation; intolerant of feeding, with nausea or vomiting
Exam
tympanic, distended abdomen; hyperactive bowel sounds that become absent in advanced stages; abdominal rebound, guarding, and/or rigidity if perforation or close to perforation; empty rectum; incarcerated femoral, obturator, umbilical, or ventral hernia may be present
1st investigation
- abdominal x-ray:
gaseous distension of large bowel; volvulus suggested by kidney-bean-shape bowel loop
More
Other investigations
- abdominal ultrasound:
may demonstrate focal area causing obstruction (e.g., intussusception)
More - lower gastrointestinal (GI) contrast study:
may indicate site of obstruction
More - CT scan abdomen and pelvis:
gaseous distension of large bowel; may demonstrate a transition zone of obstruction
More - flexible/rigid sigmoidoscopy:
flood of stool and mucus upon passing and decompressing apex of volvulus
More
Necrotising enterocolitis
History
premature neonate weighing less than 1500 g; feeding intolerance, apnoea, lethargy, bloody stools
Exam
abdominal distension, tenderness, abdominal wall erythema, haematochezia, bradycardia
1st investigation
Other investigations
- abdominal ultrasound:
fluid collections, ascites
More
Peptic ulcer disease
History
non-steroidal anti-inflammatory drug use; family history of peptic ulcer disease; weight loss, vomiting, anorexia, and intermittent epigastric pain, usually related to eating meals; pain often nocturnal and usually relieved by antacids; melaena and/or haematemesis if erosion into blood vessel
Exam
unremarkable or epigastric tenderness, melaena, or occult bleeding on stool haemoccult test
1st investigation
- FBC:
normal or leukocytosis; anaemia present if sustained blood loss
- erect chest x-ray:
usually normal
More - upper gastrointestinal series with water-soluble contrast:
mucosal defect(s) consistent with ulcer or free intraperitoneal contrast consistent with perforation
More - upper gastrointestinal endoscopy:
mucosal inflammation, ulceration, and haemorrhage
More
Other investigations
- Helicobacter pylori breath test or stool antigen test:
positive result if Helicobacter pylori present
More
Coeliac disease
History
recurrent abdominal pain, cramping, or distension; bloating and diarrhoea; dermatitis herpetiformis, an intensely pruritic papulovesicular rash that affects the extensor limb surfaces, almost universally occurs in association with coeliac disease; may be a history of immunoglobulin A deficiency, type 1 diabetes, autoimmune thyroid disease, Down syndrome, Sjogren syndrome, inflammatory bowel disease, or primary biliary cholangitis; may be a family history of coeliac disease
Exam
generalised abdominal pain or bloating; underweight or failing to thrive; aphthous stomatitis; dermatitis herpetiformis
1st investigation
- immunoglobulin A-tissue transglutaminase (IgA-tTG):
titre above normal range for laboratory
More - quantitative immunoglobulin A (IgA):
titre normal or below normal range for laboratory
More - FBC:
may show iron deficiency anaemia
- endoscopy and small bowel biopsy:
presence of intra-epithelial lymphocytes, villous atrophy, and crypt hyperplasia
More
Viral hepatitis
History
birth or residence in endemic area, antenatal exposure, family history of chronic viral hepatitis, multiple sexual partners, sexual intercourse with infected individuals (hepatitis B and/or C), travel to developing countries, pregnant (hepatitis E); early disease: malaise, muscle and joint aches, fever, nausea, vomiting, diarrhoea, headache, anorexia, dark urine, pale stool, abdominal pain; late disease: weight loss, easy bruising and bleeding tendencies
Exam
jaundice; early disease: tender hepatosplenomegaly, lymphadenopathy; late disease: generalised wasting, cachexia, gynaecomastia, ascites, altered sensorium, asterixis, or decreased deep tendon reflexes, caput medusa, ascites, hepatosplenomegaly, congestion secondary to right heart failure
1st investigation
- serum LFTs:
high direct bilirubin, AST, ALT, alk phos and gamma-GT
More - serum IgM anti-HAV:
positive if acute hepatitis A infection
- serum hepatitis B surface antigen (HBsAg):
positive if hepatitis B infection
More - serum hepatitis B core antigen (HBcAg):
positive if hepatitis B infection
More - serum hepatitis B e antigen (HBeAg):
positive if hepatitis B infection
More - serum HCV RNA:
positive if hepatitis C infection
More - serum total (IgM and IgG) anti-HDV antibodies:
positive if hepatitis D infection
More - serum anti-HEV IgM antibodies:
positive if acute hepatitis E infection
Biliary dyskinesia
History
history of previous negative work-up for cholelithiasis common; recurrent right upper quadrant (RUQ) pain; nausea and vomiting; symptoms may or may not be associated with eating
Exam
may be equivocal; RUQ tenderness
1st investigation
- LFTs:
normal aspartate aminotransferase, alanine aminotransferase, alk phos, and bilirubin
- RUQ ultrasound:
normal
More
Other investigations
- hepatobiliary iminodiacetic acid (HIDA) scan:
decreased (<35%) gallbladder ejection fraction
More
Acute pancreatitis
History
nausea, vomiting, epigastric pain radiating to back; acute-onset abdominal pain
Exam
epigastric or upper abdominal tenderness; tachycardia and hypotension in severe cases; discoloration around the umbilicus (positive Cullen's sign) or flanks (positive Grey-Turner's sign) in cases of haemorrhagic pancreatitis; small children may demonstrate increased irritability and abdominal distension only
1st investigation
Other investigations
Splenic infarction/cysts
History
varied; may be history of trauma; cysts either asymptomatic or dull, left-sided abdominal pain; infarction typically causes fever as well as pain, but occasionally asymptomatic; left-sided shoulder and/or chest pain; presence of risk factors for splenic infarction (sickle cell disease, high altitude)
Exam
may be vague left upper quadrant tenderness
1st investigation
- Doppler ultrasound:
infarction or cyst on spleen
More
Other investigations
- CT scan abdomen with intravenous contrast:
infarction or cyst on spleen
More
Nephrolithiasis
History
family history of nephrolithiasis and/or gout; intermittent, severe, colicky flank and/or abdominal pain; nausea and vomiting; gross or microscopic haematuria; urinary frequency/urgency; atypical presentation common in younger children
Exam
ipsilateral costovertebral angle and flank tenderness; tachycardia and hypotension in pain-controlled patient may suggest concurrent urosepsis
1st investigation
Sepsis
History
may be history of decreased activity, carer concern that child is not behaving as normal; may not wake or may be difficult to rouse
Exam
fever may be present (although core temperature may also be normal or low), tachycardia, raised respiratory rate, may be delayed capillary refill time, oxygen saturations may be <92% in air, altered mental state, petechiae or purpura may be present
1st investigation
- FBC:
WBC variable; may be thrombocytopenia
More - blood glucose:
may be hypo- or hyperglycaemia
- serum electrolytes:
deranged
- blood lactate:
raised
More - arterial blood gas:
hypoxaemia and/or hypercarbia; large base deficit
- coagulation studies:
may be abnormal
- LFTs:
may be abnormal
- blood culture:
may be growth of bacteria identifying pathogen
- chest x-ray:
may reveal evidence of pneumonia
- urinalysis:
may be positive for nitrites and leukocytes if urinary tract infection present
- urine culture:
may be positive if urinary tract infection present
Testicular torsion
History
acute-onset testicular pain; nausea, and vomiting; history of recurrent episodes suggests repeated episodes of testicular torsion followed by spontaneous detorsion; history of trauma may be present
Exam
tender, oedematous testicle; affected testicle may appear higher than unaffected testicle with horizontal lie; associated scrotal erythema and oedema; absent cremasteric reflex; usually no pain relief with elevation of the scrotum; thin skin of the scrotum sometimes allows visualisation of the torsed appendage ('blue dot or black dot sign')
1st investigation
- Testicular Workup for Ischemia and Suspected Torsion (TWIST) score:
low risk (score 0 to 2), intermediate risk (3 to 4), or high risk (5 to 7)
More - duplex Doppler ultrasound of scrotum:
presence of fluid and the whirlpool sign (the swirling appearance of the spermatic cord from torsion as the ultrasound probe scans downwards perpendicular to the spermatic cord); absent or decreased blood flow in the affected testicle; decreased flow velocity in the intratesticular arteries, increased resistive indices in the intratesticular arteries
More
Other investigations
- urinalysis:
usually normal, but can be abnormal in some cases
More
Ovarian torsion
History
acute onset of one-sided lower abdominal or pelvic pain; nausea and vomiting common; history of frequent, similar episodes; fever rare
Exam
tender pelvic mass (adnexal); in patients old enough to undergo pelvic examination, cervical motion tenderness may be elicited; typically no vaginal discharge, but may be some mild to moderate vaginal bleeding
1st investigation
- pelvic ultrasound:
solid appearance of the ovary, unilateral ovarian enlargement, ovarian peripheral cystic structures, marked stromal oedema, fluid in the pouch of Douglas
Ruptured ovarian cyst
History
rupture usually spontaneous, can follow history of trauma or sexual intercourse; mild chronic lower abdominal discomfort may suddenly intensify; may occur in conjunction with torsion
Exam
adnexal tenderness; adnexal size unremarkable due to collapsed cyst; peritonism may be present in lower abdomen and pelvis
1st investigation
- pelvic ultrasound:
complex mass appearance; fluid in the pouch of Douglas
More
Other investigations
Pelvic inflammatory disease (PID)
History
sexually active; multiple partners; history may be suggestive of sexual abuse (particularly if young child); pain worse with sexual intercourse; dull, aching lower abdominal pain with or without dysuria; vaginal discharge, low-grade fever
Exam
temperature >38.3°C (101°F); cervical motion tenderness, adnexal or uterine tenderness, vaginal or cervical mucopurulent discharge
1st investigation
Other investigations
- pelvic ultrasound:
normal or may demonstrate endometritis, hydrosalpinx, pyosalpinx, tubo-ovarian abscess
More - HIV serology:
positive or negative
More - hepatitis studies:
positive or negative
More - rapid plasma reagin (RPR):
positive or negative
More - FBC:
leukocytosis
More - C-reactive protein or erythrocyte sedimentation rate:
raised
More - laparoscopy:
normal or may demonstrate endometritis, hydrosalpinx, pyosalpinx, tubo-ovarian abscess
More
Pregnancy complications
History
history of previous ectopic pregnancy or miscarriage, fallopian tube or pelvic surgery, pelvic inflammatory disease; lower abdominal pain, amenorrhoea, and vaginal bleeding
Exam
minimal abdominal tenderness and/or vaginal bleeding; pelvic examination may reveal a mass, eliciting cervical motion tenderness if haemoperitoneum is present; tubal rupture can cause haemodynamic instability
1st investigation
Other investigations
- blood type and screen:
variable
More
Empyema
History
recent pneumonia, fever, cough, chest pain; malaise, anorexia, weight loss, or fatigue may occur; presence of risk factors (immunocompromise, comorbidities predisposing to the development of pneumonia, pre-existing lung disease, iatrogenic interventions in the pleural space, male sex)
Exam
febrile, toxic patient, dullness on percussion, absence of breath sounds over affected area; abdominal tenderness and distension without guarding or rebound
1st investigation
Use of this content is subject to our disclaimer