Summary
Definition
History and exam
Key diagnostic factors
- calf swelling
- localized pain along deep venous system
Other diagnostic factors
- asymmetric edema
- prominent superficial veins
- swelling of the entire leg
- phlegmasia cerulea dolens
Risk factors
- recently bed-bound for 3 days or more
- major surgery within the preceding 3 months
- medical hospitalization within the preceding 2 months
- active cancer
- previous venous thromboembolic event
- recent trauma or fracture
- increasing age
- pregnancy and the postpartum
- varicose veins
- paralysis of the lower extremities
- hereditary thrombophilias
- factor V Leiden
- prothrombin gene G20210A mutation
- protein C or protein S deficiency
- antithrombin deficiency
- antiphospholipid syndrome
- medical comorbidity
- use of specific drugs
- obesity
- cigarette smoking
- recent long-duration air travel
- family history of venous thromboembolism
- central venous catheterization
Diagnostic tests
1st tests to order
- Wells score
- quantitative D-dimer level
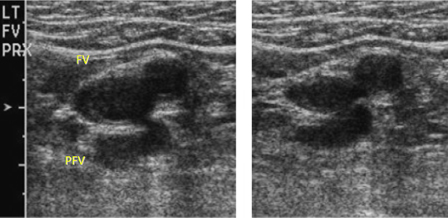
- venous duplex ultrasound (DUS)
- INR and activated partial thromboplastin time (aPTT)
- BUN and creatinine
- LFTs
- CBC
Tests to consider
- Doppler venous flow testing
- CT abdomen and pelvis with contrast
- thrombophilia screen
Treatment algorithm
suspected or confirmed DVT of the leg with phlegmasia cerulea dolens
suspected or confirmed DVT without phlegmasia cerulea dolens and no contraindications to anticoagulation: initiation-phase therapy
suspected or confirmed DVT without phlegmasia cerulea dolens: contraindications to anticoagulation
confirmed DVT of the leg: treatment-phase therapy
provoked DVT: extended-phase therapy
unprovoked DVT: extended-phase therapy
pregnant: extended-phase therapy
cancer-associated: extended-phase therapy
recurrent VTE: extended-phase therapy
Contributors
Expert advisers
Scott M. Stevens, MD
Director
Thrombosis Clinic
Intermountain Medical Center
Murray
Professor of Medicine
Department of Medicine
Intermountain Healthcare and University of Utah
Salt Lake City
UT
Disclosures
SMS declares that he has no competing interests.
Scott C. Woller, MD
Director
Thrombosis Clinic
Intermountain Medical Center
Murray
Professor of Medicine
Department of Medicine
Intermountain Healthcare and University of Utah
Salt Lake City
UT
Disclosures
SCW declares that he is expecting to receive funding of an investigator-initiated grant from Janssen Pharmaceuticals to Intermountain Health with no direct compensation to himself for research in the sum of $500,000 in 2024.
Gabriel V. Fontaine, PharmD, MBA, BCPS
Clinical Pharmacy Manager
Critical Care and Emergency Medicine
Advanced Clinical Pharmacist
Neuroscience Critical Care
Intermountain Medical Center
Murray
UT
Disclosures
GVF has received consulting fees and honoraria from AstraZeneca, Chiesi, and Anticoagulation Forum.
Acknowledgements
Dr Scott M. Stevens, Dr Scott C. Woller, and Dr Gabriel V. Fontaine would like to gratefully acknowledge Dr Geno Merli, Dr Taki Galanis, Dr Luis Eraso, Dr Geoffrey Ouma, Dr Richard White, and Dr Windsor Ting, the previous contributors to this topic.
Disclosures
GM has received grant or research support from BMS, J&J, Sanofi-Aventis, Portola, and Janssen; he has served as a Scientific Consultant for BMS, J&J, and Sanofi-Aventis. RW declares participation in numerous multicentered clinical trials sponsored by companies: Agenix, Boehringer-Ingelheim, Amgen, Bayer, Bristol-Meyer-Squibb, Novartis, Hemosense. TG, LE, GO, and WT declare that they have no competing interests.
Peer reviewers
Beverly Hunt, FRCP, FRCPath, MD
Professor of Thrombosis & Haemostasis
King's College
Consultant
Departments of Haematology, Pathology & Rheumatology
Lead in Blood Sciences
Guy's & St Thomas' NHS Foundation Trust
London
UK
Disclosures
BH declares that she has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Stevens SM, Woller SC, Kreuziger LB, et al. Antithrombotic therapy for VTE disease: second update of the CHEST guideline and expert panel report. Chest. 2021 Dec;160(6):e545-608.Full text Abstract
Mazzolai L, Ageno W, Alatri A, et al. Second consensus document on diagnosis and management of acute deep vein thrombosis: updated document elaborated by the ESC Working Group on aorta and peripheral vascular diseases and the ESC Working Group on pulmonary circulation and right ventricular function. Eur J Prev Cardiol. 2022 May 27;29(8):1248-63.Full text Abstract
Kahn SR, Lim W, Dunn AS, et al. Prevention of VTE in nonsurgical patients: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians evidence-based clinical practice guidelines. Chest. 2012 Feb;141(2 suppl):e195S-226S.Full text Abstract
Stevens SM, Woller SC, Baumann Kreuziger L, et al. Antithrombotic therapy for VTE disease: compendium and review of CHEST guidelines 2012-2021. Chest. 2024 Aug;166(2):388-404.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Cellulitis
- Calf muscle tear/Achilles tendon tear
- Calf muscle hematoma
More DifferentialsGuidelines
- NCCN clinical practice guidelines in oncology: cancer-associated venous thromboembolic disease
- ACR-AIUM-SPR-SRU practice parameter for the performance of peripheral venous ultrasound examination
More GuidelinesCalculators
Pretest Probability of Heparin Induced Thrombocytopenia (4-T's score)
More CalculatorsPatient information
Deep vein thrombosis
DVT and long-distance travel
Больше Patient informationВойдите в учетную запись или оформите подписку, чтобы получить полноценный доступ к BMJ Best Practice
Использование этого контента попадает под действие нашего заявления об отказе от ответственности