Summary
Differentials
Common
- Vaginitis and vulvovaginitis
- Herpes simplex infection
- Vaginal atrophy
- Iatrogenic
- Primary inadequate lubrication
- Vestibulodynia/vulvodynia
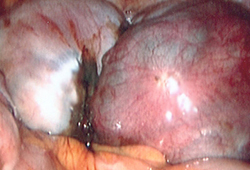
- Endometriosis
- Adenomyosis
- Leiomyomas
Uncommon
- Interstitial cystitis
- Urinary tract infections, female
- Bartholin gland abscess
- Seminal plasma hypersensitivity
- Dermatitis, contact
- Dermatitis, atopic
- Bartholin gland mass
- Imperforate hymen
- Traumatic perineal injuries
- Vulvar dystrophies
- Vaginismus
- Psychosexual disorder
- Cervicitis
- Pelvic inflammatory disease
- Hydrosalpinx
- Levator ani spasm
Contributors
Authors
Kai J. Buhling, MD, PhD
Professor
Head of Department of Gynecological Endocrinology and Reproductive Medicine
University Hospital Hamburg-Eppendorf
Hamburg
Germany
Disclosures
KJB declares that he has no competing interests.
Acknowledgements
Dr Buhling would like to gratefully acknowledge Dr Hans-Joachim Ahrendt, Dr Suketu M. Mansuria and Dr Amy N. Broach, the previous contributors to this topic.
Disclosures
SMM declares that he has no competing interests.
Peer reviewers
Lori A. Brotto, PhD, R Psych
Assistant Professor
Department of Obstetrics and Gynecology
University of British Columbia
Vancouver
Canada
Disclosures
LAB declares that she has no competing interests.
Katherine E. Bunge, MD
Clinical Instructor
Magee-Womens Hospital
University of Pittsburgh
Pittsburgh
PA
Disclosures
KEB declares that she has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
IsHak WW, Tobia G. DSM-5 changes in diagnostic criteria of sexual dysfunctions. Reprod Sys Sexual Disorders 2013;2:122.
National Institute for Health and Care Excellence. Endometriosis: diagnosis and management. Nov 2024 [internet publication].Full text
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Use of this content is subject to our disclaimer