Summary
Definition
History and exam
Key diagnostic factors
- loss or deterioration of central vision
- flashes of light
- loss of peripheral visual field
Other diagnostic factors
- floaters
Risk factors
- posterior vitreous detachment
- increasing age
- myopia
- previous cataract surgery
- trauma
- previous ophthalmic surgery
- intraocular tumor
- vitreous hemorrhage
- affected fellow eye
- diabetes mellitus
- retinopathy of prematurity
- ocular inflammation/infection
- peripheral retinal degeneration
- anatomic abnormality
- age-related macular degeneration
- phosphodiesterase-5 inhibitor use in men
- genetic and vascular causes in childhood
- childhood tumors
Diagnostic tests
1st tests to order
- visual acuity testing
- slit-lamp exam
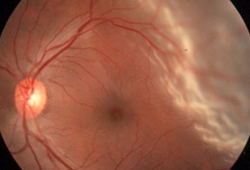
- indirect ophthalmoscopy
Tests to consider
- wide-field color photography
- optical coherence tomography (affected eye)
- B-scan ultrasonography (affected eye)
- CT/MRI of orbit
Treatment algorithm
posterior vitreous detachment without break/tear
retinal hole/tear without detachment
rhegmatogenous RD
tractional RD
exudative RD
hemorrhagic RD
Contributors
Authors
Ferenc Kuhn, MD, PhD
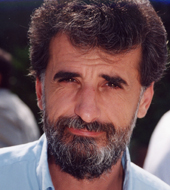
Director of Clinical Research
Helen Keller Foundation for Research and Education
Associate Professor of Ophthalmology
University of Alabama at Birmingham
Birmingham
AL
Consultant and Chief Vitreoretinal Surgeon
Department of Ophthalmology
University of Pécs Medical School
Pécs
Hungary
Disclosures
FK declares that he has no competing interests.
Acknowledgements
Dr Kuhn would like to gratefully acknowledge Dr Robert Morris, a previous contributor to this monograph. RM declares that he has no competing interests.
Peer reviewers
David Steel, MBBS, FRCOphth
Consultant Ophthalmologist
Sunderland Eye Infirmary
Sunderland
UK
Disclosures
DS declares that he has no competing interests.
Michael W. Stewart, MD
Professor and Chairman of Ophthalmology
Mayo Clinic
Jacksonville
FL
Disclosures
MWS declares that he has no competing interests.
Ron Adelman, MD, MPH, FACS
Associate Professor of Ophthalmology
Yale University School of Medicine
New Haven
CT
Disclosures
RA declares that he has no competing interests.
Scott Fraser, MD, FRCS (Ed), FRCOphth
Consultant Ophthalmologist
Sunderland Eye Infirmary
Sunderland
UK
Disclosures
SF declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Kim SJ, Bailey ST, Kovach JL, et al. Posterior vitreous detachment, retinal breaks, and lattice degeneration preferred practice pattern®. Ophthalmology. 2025 Apr;132(4):P163-96.Full text
American Academy of Ophthalmology. Referral of persons with possible eye diseases or injury - 2014. Apr 2014 [internet publication].Full text
Hikichi T, Trempe CL. Relationship between floaters, light flashes, or both, and complications of posterior vitreous detachment. Am J Ophthalmol. 1994;117:593-8. Abstract
Znaor L, Medic A, Binder S, et al. Pars plana vitrectomy versus scleral buckling for repairing simple rhegmatogenous retinal detachments. Cochrane Database Syst Rev. 2019 Mar 8;(3):CD009562.Full text Abstract
Sena DF, Kilian R, Liu SH, et al. Pneumatic retinopexy versus scleral buckle for repairing simple rhegmatogenous retinal detachments. Cochrane Database Syst Rev. 2021 Nov 11;(11):CD008350.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Vitreomacular traction
- Retinoschisis
- Diabetic retinopathy
More DifferentialsGuidelines
- Posterior vitreous detachment, retinal breaks, and lattice degeneration preferred practice pattern®
- Retina summary benchmarks - 2024
More GuidelinesPatient information
Macular degeneration
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer