Summary
Definition
History and exam
Key diagnostic factors
- at-risk demographic
- family history of SCID, infant death, or consanguinity
- recurrent and unusually severe infections
- chronic diarrhea
- failure to thrive
- absent lymphoid tissue
Other diagnostic factors
- rash
- oral or genital ulcers
- microcephaly
- skeletal abnormalities
- blindness
- dystonia
- radiation sensitivity
Risk factors
- Family history of SCID
- Family history of infant death
- Athabascan-speaking Native American people
- Consanguinity
Diagnostic tests
1st tests to order
- CBC
- flow cytometry
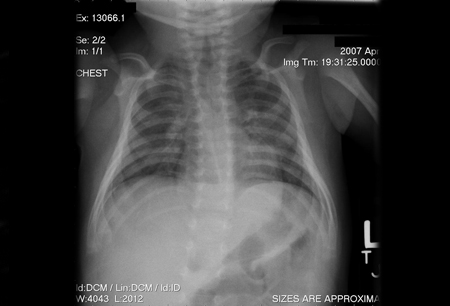
- chest x-ray
- quantitative immunoglobulin test (IgG, IgM, and IgA)
Tests to consider
- chest ultrasound
- CT scan of the chest
- MRI chest
- fundoscopy
- enzyme testing
- serum uric acid
- T-cell proliferation studies
- polymerase chain reaction-based viremia testing
- radiation sensitivity of fibroblast cultures
- genetic testing
Treatment algorithm
confirmed SCID
Contributors
Authors
Javier Chinen, MD, PhD
Professor
Pediatrics, Allergy, and Immunology
Baylor College of Medicine
Texas Children’s Hospital
Houston
TX
Disclosures
JC declares that he has no competing interests.
Acknowledgements
Dr Chinen would like to gratefully acknowledge Dr John M. Cunningham, Dr James L. LaBelle, Dr John Routes, Dr James Verbsky, Dr Nicole Chase, and Dr Ebrahim Shakir, the previous contributors to this topic.
Disclosures
JLL, JR, JV, and NC are authors of references cited in this topic. JMC and ES declare that they have no competing interests.
Peer reviewers
Elizabeth Secord, MD
Professor of Pediatrics
Division of Immunology
Wayne State University School of Medicine
Detroit
MI
Declarações
ES declares that she has no competing interests.
Waseem Qasim, BMedSci (Hons), MBBS, MRCP (UK), MRCPCH, PhD
Senior Lecturer
Institute of Child Health
Consultant in Paediatric Immunology & Bone Marrow Transplantation
Great Ormond Street Hospital
London
UK
Declarações
WQ declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Bousfiha A, Moundir A, Tangye SG, et al. The 2022 update of IUIS phenotypical classification for human inborn errors of immunity. J Clin Immunol. 2022 Oct 6 [Epub ahead of print]. Resumo
Tangye SG, Al-Herz W, Bousfiha A, et al. Human inborn errors of immunity: 2022 update on the classification from the International Union of Immunological Societies Expert Committee. J Clin Immunol. 2022 Jun 24;1-35 [Epub ahead of print].Texto completo Resumo
Bonilla FA, Khan DA, Ballas ZK, et al. Practice parameter for the diagnosis and management of primary immunodeficiency. J Allergy Clin Immunol. 2015 Nov;136(5):1186-205.e1-78.Texto completo Resumo
Buckley RH. Molecular defects in human severe combined immunodeficiency and approaches to immune reconstitution. Ann Rev Immunol. 2004:22:625-55. Resumo
Heimall J, Buckley RH, Puck J, et al. Recommendations for screening and management of late effects in patients with severe combined immunodeficiency after allogenic hematopoietic cell transplantation: a consensus statement from the second pediatric blood and marrow transplant consortium international conference on late effects after pediatric HCT. Biol Blood Marrow Transplant. 2017 Aug;23(8):1229-40.Texto completo Resumo
Candotti F, de Villartay JP, Moshous D, et al. Severe combined immune deficiency. In: Sullivan KE, Stiehm ER, eds. Stiehm’s immune deficiencies: inborn errors in immunity. 2nd ed. Cambridge, MA: Academic Press, 2020:153-205.
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- 22q11.2 Microdeletion Syndrome/DiGeorge syndrome
- Omenn syndrome
- Zeta chain-associated protein 70 deficiency
Mais Diagnósticos diferenciaisDiretrizes
- Recommendations for screening and management of late effects in patients with severe combined immunodeficiency after allogeneic hematopoietic cell transplantation
- Practice parameter for the diagnosis and management of primary immunodeficiency
Mais DiretrizesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal