Summary
Definition
History and exam
Key diagnostic factors
- history of repetitive jobs or overhead hobbies/activities
- pain in upper extremity and adjacent areas
- paresthesias in arms, hands, and/or fingers
- circulatory changes in upper extremity
- upper extremity fatigue
Other diagnostic factors
- history of clavicular fracture
- palpation of cervical rib
- subcutaneous venous collateral distention around shoulders (Urschel sign)
- motor weakness
- hyperhidrosis
- thenar eminence muscle atrophy
- exertional pain/claudication
- supraclavicular systolic bruit
- blood pressure difference between extremities
- positive Adson (scalene) test
- positive costoclavicular test
- positive hyperabduction test
- positive elevated arm stress test (Roos test)
- positive stretch test
- positive upper limb tension tests
- positive Wright maneuver
- edema/swelling of upper extremity
Risk factors
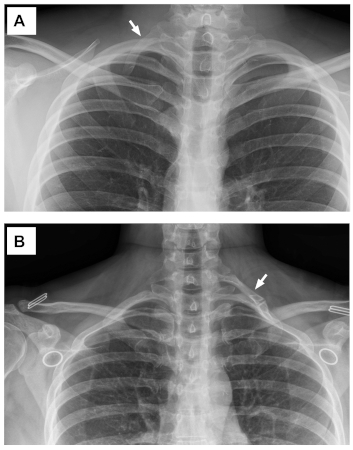
- cervical ribs (partial or complete)
- abnormal (hypoplastic) first rib or bony abnormalities
- anomalies of muscular development (interdigitation, scalene minimis muscle)
- fibro-fascial or ligamentous bands
- fractures of clavicle or first rib
- overdevelopment of muscles (bodybuilding, heavy labor with upper extremities)
- traumatic injuries (whiplash, upper extremity distraction injuries)
Diagnostic tests
1st tests to order
- CXR
- cervical spine x-ray
- electrodiagnostic testing (nerve conduction velocity and electromyography)
- duplex ultrasonography
- contrast venography, catheter-directed therapy
- CT angiography
Tests to consider
- MRI neck/clavicle/shoulder
- muscle block
- conventional arteriography
- magnetic resonance angiography (MRA)
- magnetic resonance venography (MRV)
- CBC, coagulation, and thrombophilia studies
Treatment algorithm
neurogenic TOS (NTOS)
venous TOS (vTOS)
arterial TOS (ATOS)
neurovascular (combined)
Contributors
Authors
Robert W. Thompson, MD
Center for Thoracic Outlet Syndrome
Department of Surgery (Section of Vascular Surgery)
Washington University School of Medicine and Barnes-Jewish Hospital
St. Louis
MO
Disclosures
RWT is an author of several references cited in this topic, has coauthored articles with other authors on this topic, has contributed to educational events on this topic, has provided expert witness testimony on this topic, and has directed use of philanthropic funds received by Washington University School of Medicine to support staff for research on this topic.
Hugh A. Gelabert, MD
Division of Vascular Surgery
Gonda (Goldschmied) Vascular Center
David Geffen School of Medicine at UCLA
Los Angeles
CA
Disclosures
HAG is an author of several references cited in this topic, has coauthored articles with other authors on this topic, has contributed to educational events on this topic, has provided expert witness testimony on this topic, and has directed use of philanthropic funds received by University of California Los Angeles School of Medicine to support research on this topic.
Joep A. W. Teijink, MD
Department of Vascular Surgery
Catharina Hospital
Eindhoven
The Netherlands
Department of Epidemiology
CAPHRI School for Public Health and Primary Care
Faculty of Health, Medicine and Life Sciences
Maastricht University
Maastricht
The Netherlands
Disclosures
JAWT is coauthor of several references cited in this topic, has contributed to educational events on this topic, and has provided expert witness testimony on this topic. No financial disclosures.
Acknowledgements
Dr Robert W. Thompson, Dr Joep A.W. Teijink, and Dr Hugh A. Gelaber would like to gratefully acknowledge Dr Chaney Stewman, Dr Marc I. Harwood, Dr Pedro K. Beredjiklian, Dr Peter C. Vitanzo, Dr Harold C. Urschel Jr, Rachel Montano, and Brenda Knee, previous contributors to this topic. CS is the author of a reference cited in this topic. MIH is the author of a reference cited in this topic. PKB has stock ownership in Wright Medical Inc. PCV is the author of a reference cited in this topic. HCU is an author of several references cited in this topic. RM and BK declare that they have no competing interests.
Peer reviewers
Ian Loftus, BSc, MB, ChB, FRCS, MD
Professor of Vascular Surgery
St. George's NHS Healthcare Trust
London
UK
Disclosures
IL declares that he has no competing interests.
Scott R. Laker, MD
Assistant Professor
University of Colorado School of Medicine
Aurora
CO
Disclosures
SRL is the author of a reference cited in this topic.
John A. Kern, MD
Chief
Cardiothoracic Surgery
University of Virginia School of Medicine
Charlottesville
VA
Disclosures
JAK declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Illig KA, Donahue D, Duncan A, et al. Reporting standards of the Society for Vascular Surgery for thoracic outlet syndrome. J Vasc Surg. 2016 Sep;64(3):e23-35.Full text Abstract
Vemuri C, McLaughlin LN, Abuirqeba AA, et al. Clinical presentation and management of arterial thoracic outlet syndrome. J Vasc Surg. 2017 May;65(5):1429-39.Full text Abstract
Vemuri C, Salehi P, Benarroch-Gampel J, et al. Diagnosis and treatment of effort-induced thrombosis of the axillary subclavian vein due to venous thoracic outlet syndrome. J Vasc Surg Venous Lymphat Disord. 2016 Oct;4(4):485-500.Full text Abstract
George EL, Arya S, Rothenberg KA, et al. Contemporary practices and complications of surgery for thoracic outlet syndrome in the United States. Ann Vasc Surg. 2021 Apr;72:147-58. Abstract
Peek J, Vos CG, Ünlü Ç, et al. Outcome of surgical treatment for thoracic outlet syndrome: systematic review and meta-analysis. Ann Vasc Surg. 2017 Apr;40:303-26. Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Vasospasm, embolism, or insufficiency
- Coronary artery disease
- Myocardial infarction
More DifferentialsGuidelines
- Thoracic outlet syndrome part I: systematic review of the literature and consensus on anatomy, diagnosis, and classification of thoracic outlet syndrome by the European Association of Neurosurgical Societies’ section of peripheral nerve surgery
- Thoracic outlet syndrome part II: consensus on the management of neurogenic thoracic outlet syndrome by the European Association of Neurosurgical Societies' section of peripheral nerve surgery
More GuidelinesPatient information
Raynaud phenomenon
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer