Summary
Definition
History and exam
Key diagnostic factors
- hypertension
- signs of retinopathy
- edema
Other diagnostic factors
- poor vision
- numbness of the lower extremities
- pain of the lower extremities
- constitutional symptoms (advanced disease)
- foot changes
- orthostatic hypotension
- skin changes
- muscular atrophy
- pallor (as glomerular filtration rate declines)
- bleeding tendency (advanced disease)
- Kussmaul respirations (advanced disease)
Risk factors
- sustained hyperglycemia
- hypertension
- family history of hypertension and/or kidney disease
- obesity
- smoking
- physical inactivity
- dyslipidemia
- high protein, fat, and sodium intake
Diagnostic investigations
1st investigations to order
- urinalysis
- urinary albumin-to-creatinine ratio (ACR)
- serum creatinine with GFR estimation
- kidney ultrasound
Investigations to consider
- cystatin C with GFR estimation
- albumin excretion rate (AER)
- CT abdomen
- magnetic resonance angiography (MRA)
- Doppler ultrasound
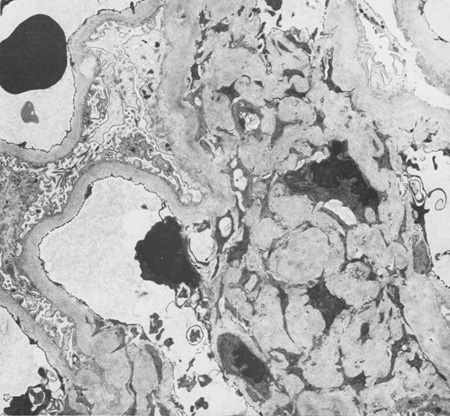
- kidney biopsy
Treatment algorithm
type 1 diabetes with nephropathy: not on dialysis
type 2 diabetes with nephropathy: not on dialysis
on peritoneal dialysis or hemodialysis
Contributors
Authors
David J. Leehey, MD, FACP

Professor of Medicine
Division of Nephrology
Loyola University Medical Center
Maywood
IL
Disclosures
DJL declares that he has no competing interests. DJL is an author of references cited in this topic.
Irfan Moinuddin, MD

Assistant Professor of Medicine
Southern Illinois University School of Medicine
Springfield
IL
Disclosures
IM declares that he has no competing interests.
Peer reviewers
Rajiv Agarwal, MD
Professor of Medicine
Department of Medicine
Division of Nephrology
Indiana University School of Medicine
Indianapolis
IN
Disclosures
RA declares that he has no competing interests.
Merlin C. Thomas, PhD
Associate Professor
Baker IDI Heart and Diabetes Institute
Melbourne
Australia
Disclosures
MCT has received honoraria for speaking and educational sessions conducted by Sanofi-Aventis, Servier, Boehringer-Ingleheim, Abbott, Amgen, and Jansen-Cilag.
Damian Fogarty, BSc, MD, FRCP
Consultant/Senior Lecturer in Renal Medicine
Belfast City Hospital and Queen's University Belfast
Belfast City Hospital
Belfast
Northern Ireland
UK
Disclosures
DF has no share options, research support, or employment with pharmaceutical companies. He has received one-time speaking fees to cover his time preparing educational talks in the broad areas of diabetic nephropathy and chronic kidney disease, promoting early recognition and evidence-based or best practice management.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
American Diabetes Association. Standards of care in diabetes - 2025. Diabetes Care. 2025 Jan;48(suppl 1):S1-344.Full text
Kidney Disease: Improving Global Outcomes (KDIGO) Diabetes Work Group. KDIGO 2022 clinical practice guideline for diabetes management in chronic kidney disease. Kidney Int. 2022 Nov;102(5s):S1-127.Full text Abstract
de Boer IH, Khunti K, Sadusky T, et al. Diabetes management in chronic kidney disease: a consensus report by the American Diabetes Association (ADA) and Kidney Disease: Improving Global Outcomes (KDIGO). Diabetes Care. 2022 Dec 1;45(12):3075-90.Full text Abstract
Davies MJ, Aroda VR, Collins BS, et al. Management of hyperglycemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2022 Nov 1;45(11):2753-86.Full text Abstract
Lo C, Toyama T, Wang Y, et al. Insulin and glucose-lowering agents for treating people with diabetes and chronic kidney disease. Cochrane Database Syst Rev. 2018 Sep 24;(9):CD011798.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Nondiabetic kidney disease
- Multiple myeloma
- Renal tract obstruction
More DifferentialsGuidelines
- Standards of care in diabetes - 2025
- Newer pharmacologic treatments in adults with type 2 diabetes
More GuidelinesPatient information
Diabetes: what can I do to keep healthy?
Chronic kidney disease: what is it?
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer