Summary
Definition
History and exam
Key diagnostic factors
- presence of risk factors
- recurrent episodes of binge eating
- recurrent inappropriate compensatory behaviour
- eating disturbance not exclusively during periods of anorexia nervosa
- depression and low self-esteem
- concern about weight and body shape
- dental erosion
- parotid hypertrophy
- Russell's sign
- arrhythmia
Other diagnostic factors
- age 20 to 35 years
- menstrual irregularity
- drug-seeking behaviour
- deliberate misuse of insulin
- self-injurious behaviour
- gastrointestinal symptoms
- history of dieting
- marked fluctuations in weight
- shoplifting behaviour
- use of ipecac
- needle marks on skin
- vomiting in pregnancy
Risk factors
- female sex
- personality disorder
- body-image dissatisfaction
- history of sexual abuse
- impulsivity
- family history of alcoholism
- family history of depression
- family history of eating disorder
- childhood overweight or obesity
- exposure to media pressure
- early onset of puberty
- urbanisation
- family history of obesity
- participation in elite-level sports
Diagnostic investigations
1st investigations to order
- serum electrolytes
- serum creatinine
- serum magnesium
- urine pregnancy test
- serum LFTs
- serum creatine kinase (CK)
- FBC
- urinalysis
Investigations to consider
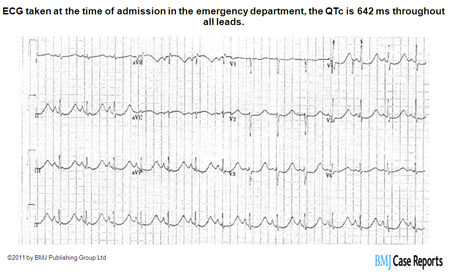
- ECG
- serum ferritin
- serum B12
- serum red blood cell folate
- dual-energy x-ray absorptiometry scan for bone density
Treatment algorithm
non-pregnant adults
children and adolescents
pregnant
Contributors
Authors
Debra L. Safer, MD
Associate Professor
Co-Director of Stanford Eating and Weight Disorders Program
Stanford University School of Medicine
Department of Psychiatry & Behavioral Sciences
Stanford
CA
Disclosures
DLS is an author of a reference cited in this topic, and receives royalties from Guilford Press for books on adapting dialectical behaviour therapy for eating disorders.
Agradecimentos
Dr Debra L. Safer would like to gratefully acknowledge Dr David C.W. Lau and Dr C. Laird Birmingham, the previous contributors to this topic.
Declarações
DCWL declares that he has no competing interests. CLB is an author of several references cited in this topic.
Revisores
Mimi Israel, MD, FRCPC
Chair of Psychiatry
McGill University
Quebec
Canada
Declarações
MI declares that she has no competing interests.
Joel Yager, MD
Professor
Department of Psychiatry
University of New Mexico School of Medicine
Albuquerque
NM
Declarações
JY is an author of a reference cited in this topic.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th ed., text revision (DSM-5-TR). Washington, DC: American Psychiatric Publishing; 2022.
Academy for Eating Disorders. Eating disorders: critical points for early recognition and medical risk management in the care of individuals with eating disorders. 2021 [internet publication].Texto completo
Lock J, La Via MC, American Academy of Child and Adolescent Psychiatry (AACAP) Committee on Quality Issues (CQI). Practice parameter for the assessment and treatment of children and adolescents with eating disorders. J Am Acad Child Adolesc Psychiatry. 2015 May;54(5):412-25.Texto completo Resumo
Carl RL, Johnson MD, Martin TJ; Council on Sports Medicine and Fitness. Promotion of healthy weight-control practices in young athletes. Pediatrics. 2017 Sep;140(3): e20171871.Texto completo Resumo
Morgan JF, Reid F, Lacey JH. The SCOFF questionnaire: assessment of a new screening tool for eating disorders. BMJ. 1999 Dec 4;319(7223):1467-8.Texto completo Resumo
National Institute for Health and Care Excellence. Eating disorders: recognition and treatment. 16 December 2020 [internet publication].Texto completo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- Other specified feeding or eating disorder (OSFED), or unspecified feeding or eating disorder (UFED)
- Anorexia nervosa, binge-eating/purging subtype
- Binge-eating disorder
Mais Diagnósticos diferenciaisDiretrizes
- Practice guideline for the treatment of patients with eating disorders
- Eating disorders: recognition and treatment
Mais DiretrizesFolhetos informativos para os pacientes
Bulimia: what is it?
Bulimia: what are the treatment options?
Mais Folhetos informativos para os pacientesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal