Summary
Definition
History and exam
Key diagnostic factors
- acute severe chest pain
- acute severe interscapular and lower back pain
- features of Marfan syndrome
- features of Ehlers-Danlos syndrome
- left/right blood pressure differential
- pulse deficit
- diastolic murmur
- syncope
- hypotension
Other diagnostic factors
- hypertension
- dyspnea
- altered mental status
- paraplegia
- hemiparesis/paresthesia
- abdominal pain
- limb pain/pallor
- left-sided decreased breath sounds/dullness
Risk factors
- hypertension
- atherosclerotic aneurysmal disease
- Marfan syndrome
- Ehlers-Danlos syndrome
- bicuspid aortic valve
- annuloaortic ectasia
- coarctation
- smoking
- family history of aortic disease or connective-tissue disorder
- older age
- giant cell arteritis
- overlap connective-tissue disorders
- surgical/catheter manipulation
- cocaine/amphetamine use
- heavy lifting
- pregnancy
- nondiabetic
Diagnostic investigations
1st investigations to order
- ECG
- cardiac enzymes
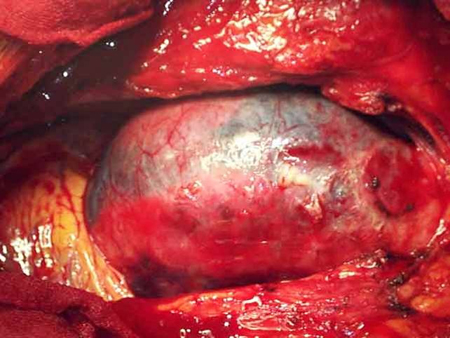
- computed tomography angiography (CTA)
- renal function tests
- liver function tests
- lactate
- complete blood count
- type and cross
Investigations to consider
- chest x-ray
- D-dimer
- transthoracic echocardiography (TTE)
- transesophageal echocardiography
- MRI
- intravascular ultrasound
Treatment algorithm
hemodynamically unstable: suspected aortic dissection
confirmed aortic dissection
chronic (all types)
Contributors
Expert advisers
Caitlin W. Hicks, MD, MS
Assistant Professor of Surgery
Division of Vascular Surgery and Endovascular Therapy
The Johns Hopkins University School of Medicine
Baltimore
MD
Disclosures
CWH receives grant funding from NIH/NIDDK, the Society for Vascular Surgery, and the American College of Surgeons; and has been reimbursed by W.L. Gore and Cook Medical for speaker engagements.
James H. Black III, MD, FACS
Chief
Vascular Surgery and Endovascular Therapy
Department of Surgery
The Johns Hopkins University School of Medicine
Baltimore
MD
Disclosures
JHB declares that he has no competing interests.
Acknowledgements
Dr Caitlin W. Hicks and Dr James H. Black III would like to gratefully acknowledge Professor Hazim J. Safi, Dr Jeffrey Wu, and Dr Eric E. Roselli, previous contributors to this topic.
Disclosures
HJS, JW, and EER declare that they have no competing interests.
Peer reviewers
Evan Lipsitz, MD
Associate Professor of Surgery
Acting Chief
Division of Vascular and Endovascular Surgery
Montefiore Medical Center and the Albert Einstein College of Medicine
Bronx
NY
Disclosures
EL declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Isselbacher EM, Preventza O, Hamilton Black J, et al. 2022 ACC/AHA guideline for the diagnosis and management of aortic disease: a report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines. J Am Coll Cardiol. 2022 Dec 13;80(24):e223-393.Full text Abstract
Mazzolai L, Teixido-Tura G, Lanzi S, et al. 2024 ESC guidelines for the management of peripheral arterial and aortic diseases. Eur Heart J. 2024 Sep 29;45(36):3538-700.Full text Abstract
Bossone E, LaBounty TM, Eagle KA. Acute aortic syndromes: diagnosis and management, an update. Eur Heart J. 2018 Mar 1;39(9):739-49d.Full text Abstract
Fleischmann D, Afifi RO, Casanegra AI, et al. Imaging and surveillance of chronic aortic dissection: a scientific statement from the American Heart Association. Circ Cardiovasc Imaging. 2022 Mar;15(3):e000075.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Acute coronary syndrome
- Pericarditis
- Aortic aneurysm
More DifferentialsGuidelines
- 2022 ACC/AHA guideline for the diagnosis and management of aortic disease
- 2021 AHA/ACC/ASE/CHEST/SAEM/SCCT/SCMR guideline for the evaluation and diagnosis of chest pain
More GuidelinesPatient information
Aortic dissection
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer