Summary
Definition
History and exam
Key diagnostic factors
- persistent low back pain
- radicular leg pain
- activity-related symptoms
Other diagnostic factors
- restriction in lumbar motion
- positive straight leg raise
- neurological deficit (leg weakness, sensory loss, bladder and bowel symptoms)
Risk factors
- increasing age
- genetic influence
- occupation (excessive axial loads, vibrations from transportation)
- tobacco smoking
- facet joint tropism and arthritis
- abnormal pelvic morphology
- changes in sagittal alignment
- obesity
- diabetes mellitus
- atherosclerosis
Diagnostic tests
1st tests to order
- erect lumbar spine x-ray
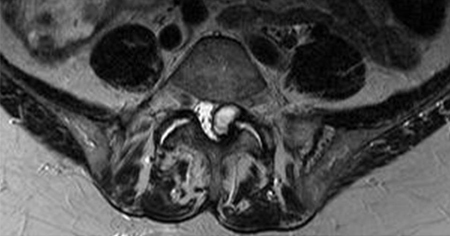
- MRI spine
Tests to avoid
- dermatomal somatosensory evoked potentials
- nerve conduction studies
Tests to consider
- CT spine
- flexion/extension spine x-rays
- single photon emission computed tomography
- CT myelogram
- discography
- MRI with gadolinium (contrast)
Treatment algorithm
neurological emergency (nerve root deficit or cauda equina syndrome)
acute back pain: <3 months duration from initial presentation or exacerbation of chronic pain
chronic back pain: ≥3 months duration from initial presentation
Contributors
Authors
Jwalant S. Mehta, MBBS, MS(Orth), D(Orth), MCh(Orth), FRCS(Orth)
Consultant Spine Surgeon
Royal Orthopaedic Hospital
Birmingham
UK
Disclosures
JSM declares that he has received research support from Stryker K2M, Depuy Synthes and Nuvasive; is a speaker for AO Spine and Scoliosis Research Society; serves on the editorial board for the European Spine Journal, the Spine Deformity Journal, and the Bone Joint Journal, is a reviewer for the Global Spinal Journal, and is part of the Paediatric Spine Study Group.
Acknowledgements
Dr Jwalant S. Mehta would like to gratefully acknowledge Dr Giannoulis Kyriakos and Dr Nasir Quiraishi, previous contributors to this topic. GK and NQ declare that they have no competing interests.
Peer reviewers
Jayesh Trivedi, FRCS (Orth)
Consultant Spine Surgeon and Head of Department
Centre for Spinal Studies
Robert Jones and Agnes Hunt Hospital NHS Foundation Trust
Oswestry
Alder Hey University Children's Hospital
Liverpool
UK
Disclosures
JT declares that he has no competing interests.
John Ratliff, MD, FAANS, FACS
Associate Professor
Department of Neurosurgery
Stanford University
Stanford
CA
Disclosures
JR declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Kreiner DS, Hwang SW, Easa JE, et al. An evidence-based clinical guideline for the diagnosis and treatment of lumbar disc herniation with radiculopathy. Spine J. 2014 Jan;14(1):180-91. Abstract
National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management. Dec 2020 [internet publication].Full text
Expert Panel on Neurological Imaging, Hutchins TA, Peckham M, et al. ACR Appropriateness Criteria® Low Back Pain: 2021 Update. J Am Coll Radiol. 2021 Nov;18(11s):S361-S379.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Spinal tumor
- Spinal infection
- Postural back pain
More DifferentialsGuidelines
- CDC prescribing opioids for pain
- ACR appropriateness criteria: low back pain
More GuidelinesPatient information
Back pain (lower back)
Back pain: questions to ask your doctor
More Patient informationLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer