Resumo
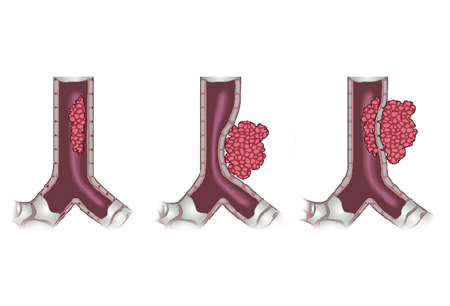
Definição
História e exame físico
Principais fatores diagnósticos
- shortness of breath
- cough
- hemoptysis
- wheeze
- stridor
Outros fatores diagnósticos
- hoarseness
- orthopnea
- dysphagia
- chest pain
- anxiety
- tachypnea
- tachycardia
- accessory muscle use
- cyanosis
- crackles
Fatores de risco
- lung cancer
- primary airway malignancy
- smoking
- artificial airways
- tracheobronchial stents
- transtracheal oxygen catheters
- lung transplantation
- neurocognitive and neuromuscular disorders
- relapsing polychondritis
- granulomatosis with polyangiitis (formerly known as Wegener granulomatosis)
- tracheobronchomalacia
- endobronchial infections
- extrathoracic and distant malignancies
Investigações diagnósticas
Primeiras investigações a serem solicitadas
- chest x-ray
Investigações a serem consideradas
- bronchoscopy (flexible and/or rigid)
- CT chest
- MRI of chest
- flow-volume loops (FVL)
- spirometry
Novos exames
- endobronchial ultrasound (EBUS)
Algoritmo de tratamento
acute presentation
subacute presentation
Colaboradores
Autores
Coral X. Giovacchini, MD
Assistant Professor of Medicine
Department of Internal Medicine
Division of Pulmonary, Allergy & Critical Care Medicine
Duke University Hospital
Durham
NC
Declarações
CXG declares that she has no competing interests.
Michael Dorry, MD
Clinical Associate
Department of Medicine
Duke University Hospital
Durham
NC
Declarações
MD declares that he has no competing interests.
Agradecimentos
Dr Coral X. Giovacchini and Dr Michael Dorry would like to gratefully acknowledge Dr Jose Fernando Santacruz, a previous contributor to this topic.
Declarações
JFS is a consultant for Boston Scientific and is the author of several studies referenced in this topic.
Revisores
Krishna M. Sundar, MD
Adjunct Assistant Professor
University of Utah
Director
Pulmonary & Critical Care Research
IHC Urban South Intermountain Utah Valley Pulmonary Clinic
Provo
UT
Declarações
KMS declares that he has no competing interests.
Andrew Parfitt, MBBS, FFAEM
Clinical Director
Acute Medicine
Associate Medical Director
Consultant Emergency Medicine
Guy's and St Thomas' NHS Foundation Trust
Clinical Lead and Consultant
Accident Emergency Medicine
St Thomas' Hospital
London
UK
Declarações
AP declares that he has no competing interests.
Créditos aos pareceristas
Os tópicos do BMJ Best Practice são constantemente atualizados, seguindo os desenvolvimentos das evidências e das diretrizes. Os pareceristas aqui listados revisaram o conteúdo pelo menos uma vez durante a história do tópico.
Declarações
As afiliações e declarações dos pareceristas referem--se ao momento da revisão.
Referências
Principais artigos
Murgu SD, Egressy K, Laxmanan B, et al. Central Airway Obstruction: Benign Strictures, Tracheobronchomalacia, and Malignancy-related Obstruction. Chest. 2016 Aug;150(2):426-41.Texto completo Resumo
Bolliger CT, Mathur PN, Beamis JF, et al. ERS/ATS statement on interventional pulmonology. European Respiratory Society. Eur Respir J. 2002;19:356-373.Texto completo Resumo
Mahmood K, Frazer-Green L, Gonzalez AV, et al. Management of central airway obstruction: an American College of Chest Physicians clinical practice guideline. Chest. 18 Jul 2024 [Epub ahead of print].Texto completo Resumo
Rosell A, Stratakos G. Therapeutic bronchoscopy for central airway diseases. Eur Respir Rev. 2020 Nov 18;29(158):190178.Texto completo Resumo
Ernst A, Silvestri GA, Johnstone D. Interventional pulmonary procedures: guidelines from the American College of Chest Physicians. Chest. 2003;123:1693-1717. Resumo
Artigos de referência
Uma lista completa das fontes referenciadas neste tópico está disponível para os usuários com acesso total ao BMJ Best Practice.
Diagnósticos diferenciais
- COPD exacerbation
- Asthma exacerbation
- Pneumonia
Mais Diagnósticos diferenciaisDiretrizes
- ACR appropriateness criteria: tracheobronchial disease
- Management of central airway obstruction
Mais DiretrizesFolhetos informativos para os pacientes
Bronchoscopy
Mais Folhetos informativos para os pacientesConectar-se ou assinar para acessar todo o BMJ Best Practice
O uso deste conteúdo está sujeito ao nosso aviso legal