Summary
Definition
History and exam
Key diagnostic factors
- older age
- fatigue
- exercise intolerance
- pallor
- bruising or bleeding
- prior chemotherapy and/or radiation therapy
- congenital disorder
- bacterial infections
Other diagnostic factors
- autoimmune disorders
- splenomegaly
- hepatomegaly
- lymphadenopathy
Risk factors
- age >70 years
- prior chemotherapy
- prior radiation therapy
- prior autologous hematopoietic stem cell transplantation
- congenital disorders
- tobacco exposure
- benzene exposure
- aplastic anemia
- paroxysmal nocturnal hemoglobinuria (PNH)
Diagnostic tests
1st tests to order
- CBC with differential
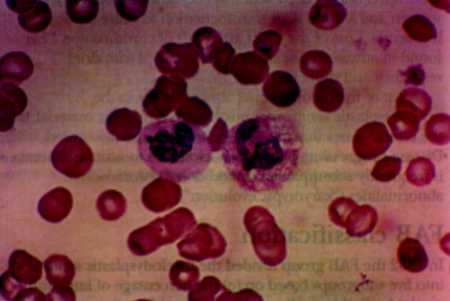
- peripheral blood smear
- reticulocyte count
- red blood cell folate
- serum vitamin B12
- iron studies
- bone marrow aspiration with iron stain
- bone marrow core biopsy
- genetic testing
Tests to avoid
- fluorescence in situ hybridization (FISH)
Tests to consider
- viral serology
- serum erythropoietin
- lactate dehydrogenase
- HLA typing
- flow cytometry
Treatment algorithm
lower-risk disease: asymptomatic
lower-risk disease: MDS-5q (del(5q) ± one other cytogenetic abnormality except those involving chromosome 7) with symptomatic anemia
lower-risk disease: MDS-SF3B1 (no del(5q) ± other cytogenetic abnormalities with ring sideroblasts ≥15% [or ≥5% with an SF3B1 mutation]) with symptomatic anemia
lower-risk disease: no del(5q) with ring sideroblasts <15% (or <5% with an SF3B1 mutation) with symptomatic anemia
lower-risk disease: with clinically relevant thrombocytopenia or neutropenia (without symptomatic anemia)
higher-risk disease: transplant candidate
higher-risk disease: nontransplant candidate
Contributors
Authors
Vijaya Raj Bhatt, MBBS, MS
Professor
Section Leader, Malignant Hematology
University of Nebraska Medical Center Division of Hematology-Oncology
Nebraska
NE
Disclosures
VRB has participated in a Safety Monitoring Committee for Protagonist Therapeutics and has served as an Associate Editor for the journal Current Problems in Cancer, and as a member of the National Comprehensive Cancer Network Acute Myeloid Leukemia panel. He has received consulting fees from Taiho, Sanofi, Imugene, Genentech, Incyte, Servier Pharmaceuticals, and AbbVie; research funding (institutional) from Cynata Therapeutics, MEI Pharma, Actinium Pharmaceutical, Sanofi, AbbVie, Pfizer, Incyte, Jazz, and NMDP; and drug support (institutional) from Chimerix for a trial.
Prajwal Dhakal, MBBS
Clinical Assistant Professor of Internal Medicine-Hematology, Oncology, and Blood and Marrow Transplantation
University of Iowa
Iowa City
IA
Disclosures
PD has received honoraria from the Aplastic Anemia and MDS International Foundation, and Iowa Oncology Society. PD has received consulting fees from AbbVie, Genentech, and Stemline Therapeutics.
Acknowledgements
Dr Vijaya Raj Bhatt and Dr Prajwal Dhakal would like to gratefully acknowledge Professor Apar Kishor Ganti and Associate Professor Alissa Marr, previous contributors to this topic.
Disclosures
AKG has received research support from Amgen, Apexigen, Bristol-Myers Squibb, Janssen, Merck, New Link Genetics, Pfizer, and Takeda Oncology. AKG has been reimbursed for consulting work for AbbVie and Genentech. None of the grants or payments relate to work involving myelodysplastic syndrome. AM declares that she has no competing interests.
Peer reviewers
David P. Steensma, MD, FACP
Associate Professor of Medicine (Hematology) and Oncology
Division of Hematology
Department of Medicine
Mayo Clinic
Rochester
MN
Disclosures
DPS declares that he has no competing interests.
Adrian C. Newland, BA, MB, BCh, MA, FRCP, FRCPath
Professor of Haematology
Queen Mary University
London
UK
Disclosures
ACN declares that he has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
Killick SB, Wiseman DH, Quek L, et al. British Society for Haematology guidelines for the diagnosis and evaluation of prognosis of adult myelodysplastic syndromes. Br J Haematol. 2021 Jul;194(2):282-93.Full text Abstract
Killick SB, Ingram W, Culligan D, et al. British Society for Haematology guidelines for the management of adult myelodysplastic syndromes. Br J Haematol. 2021 Jul;194(2):267-81.Full text Abstract
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology: myelodysplastic syndromes [internet publication].Full text
Fenaux P, Haase D, Santini V, et al; ESMO Guidelines Committee. Myelodysplastic syndromes: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021 Feb;32(2):142-56.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Aplastic anemia
- HIV infection
- Other viral infections (e.g., parvovirus, CMV, or hepatitis)
More DifferentialsGuidelines
- NCCN clinical practice guidelines in oncology: myelodysplastic syndromes
- Guidelines for the diagnosis and treatment of myelodysplastic neoplasias and chronic myelomonocytic leukemia (11th update)
More GuidelinesCalculators
Revised International Prognostic Scoring System (IPSS-R) for myelodysplastic syndrome
More CalculatorsLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer