Summary
Definition
History and exam
Key diagnostic factors
- presencia de factores de riesgo
- peso corporal significativamente bajo
- temor a ganar peso o a ponerse gordo, o comportamientos que interfieren con el aumento de peso a pesar de haber evidencias de que el peso corporal es significativamente bajo
- imagen corporal distorsionada
- restricción calórica
- atracones y/o purgas
- abuso de laxantes, diuréticos o píldoras adelgazantes
- amenorrea
- disminución de grasa subcutánea
Other diagnostic factors
- fatiga general, debilidad muscular y mala concentración
- preocupación significativa con pensamientos sobre la comida
- hipotensión ortostática
- síntomas gastrointestinales inespecíficos
- síntomas y signos cardíacos
- cambios en el pelo, la piel y las uñas
- edema postural
- osteopenia u osteoporosis
Risk factors
- sexo femenino
- adolescencia y pubertad
- rasgos obsesivos y perfeccionistas
- exposición a los medios occidentales
- influencia genética
- clases socioeconómicas media y alta
- atleta
- burlas relacionadas con la apariencia
- maltrato infantil
- enfermedad celíaca
- Diabetes mellitus de tipo 1
Diagnostic tests
1st tests to order
- diagnóstico clínico
- hemograma completo (HC)
- química sérica
- pruebas de función tiroidea
- pruebas de función hepática
- glucemia
- análisis de orina
- Prueba Sit Up-Stand-Squat (SUSS)
Tests to consider
- Cuestionario SCOFF (por sus siglas en inglés: sick, control, one, fat, food) )
- electrocardiograma (ECG)
- densitometría ósea (radioabsorciometría de doble energía)
- estradiol en las mujeres
- testosterona en los hombres
- prueba de embarazo en orina o suero
Treatment algorithm
médicamente estable y apto para el tratamiento ambulatorio
clínicamente inestable o fracaso del manejo ambulatorio
Contributors
Authors
Evelyn Attia, MD
Professor of Psychiatry
Columbia University and Weill Cornell Medical College
New York
NY
Disclosures
EA receives royalties from UpToDate and Oxford University Press for authorship and has served as a clinical advisor to Equip Health, Inc.
B. Timothy Walsh, MD
Professor of Psychiatry
Columbia University
New York
NY
Disclosures
BTW has received royalties and honoraria for writing, editing, speaking, or consulting from Guilford Publications, McGraw-Hill, Oxford University Press, UpToDate, Wiley, the University of British Columbia, Silverhill Hospital, the University of Alabama, the American Society for Clinical Psychopharmacology, Health Advances, and Dell Medical School.
Acknowledgements
Professor Evelyn Attia and Professor B. Timothy Walsh would like to gratefully acknowledge Dr Pauline S. Powers and Dr Abby M. Irwin, previous contributors to this topic.
Disclosures
PSP and AMI declare that they have no competing interests.
Peer reviewers
Heather Thompson-Brenner, MD
Director
Eating Disorders Program Center for Anxiety and Related Disorders
Psychology Department
Boston University
Boston
MA
Disclosures
HTB declares that she has no competing interests.
Peer reviewer acknowledgements
BMJ Best Practice topics are updated on a rolling basis in line with developments in evidence and guidance. The peer reviewers listed here have reviewed the content at least once during the history of the topic.
Disclosures
Peer reviewer affiliations and disclosures pertain to the time of the review.
References
Key articles
American Psychiatric Association. Diagnostic and statistical manual of mental disorders, 5th ed., text revision (DSM-5-TR). Washington, DC: American Psychiatric Publishing; 2022.
National Institute for Health and Care Excellence. Eating disorders: recognition and treatment. Dec 2020 [internet publication].Full text
American Psychiatric Association. Practice guideline for the treatment of patients with eating disorders. Feb 2023 [internet publication].Full text
Royal College of Psychiatrists. Medical emergencies in eating disorders (MEED): guidance on recognition and management. Oct 2023 [internet publication].Full text
Hornberger LL, Lane MA, Committee on Adolescence. Identification and management of eating disorders in children and adolescents. Pediatrics. 2021 Jan;147(1):e2020040279.Full text Abstract
Reference articles
A full list of sources referenced in this topic is available to users with access to all of BMJ Best Practice.
Differentials
- Bulimia nerviosa
- Trastorno de ingesta de alimentación selectiva (ARFID)
- Depresión
More DifferentialsGuidelines
- Determining treatment goal weights for children and adolescents with anorexia nervosa
- Practice guideline for the treatment of patients with eating disorders
More GuidelinesPatient information
Anorexia
Anorexia: preguntas que debe hacer a su médico
More Patient informationCalculators
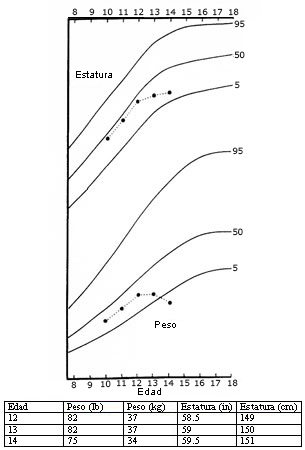
Percentiles de índice de masa corporal (IMC) para niños (entre 2 y 20 años)
Percentiles de índice de masa corporal (IMC) para niñas (entre 2 y 20 años)
More CalculatorsLog in or subscribe to access all of BMJ Best Practice
Use of this content is subject to our disclaimer